Thanks to Michael McGonigal MD for highlighting this in his excellent Trauma Professional’s Blog:
- Body temperature does not necessarily reflect brain temperature
- Low brain temperature was independently associated with a worse outcome in a recent study
- Brain temperature within the range of 36.5°C to 38°C was associated with a lower probability of death in this study
- There are no randomised studies on which to base the practice of aggressive cooling of febrile patients with traumatic brain injury
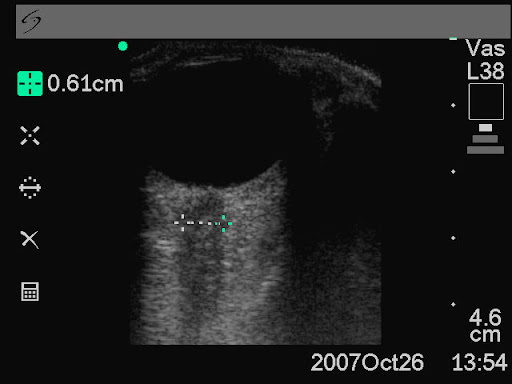
There are few prospective studies reporting the effect of spontaneous temperature changes on outcome after severe traumatic brain injury (TBI). Where studies have been conducted, results are based on systemic rather than brain temperature per se. However, body temperature is not a reliable surrogate for brain temperature. Consequently, the effect of brain temperature changes on outcome in the acute phase after TBI is not clear. Continuous intraparenchymal brain temperature was measured in consecutive admissions of severe TBI patients during the course of the first 5 days of admission to the intensive care unit (ICU). Patients received minimal temperature altering therapy during their ICU stay. Logistic regression was used to explore the relationship between the initial, the 24-h mean, and the 48-h mean brain temperature with outcome for mortality at 30 days and outcome at 3 months. Multifactorial analysis was performed to account for potential confounders. At the 24-h time point, brain temperature within the range of 36.5°C to 38°C was associated with a lower probability of death (10-20%). Brain temperature outside of this range was associated with a higher probability of death and poor 3-month neurological outcome. After adjusting for other predictors of outcome, low brain temperature was independently associated with a worse outcome. Lower brain temperatures (below 37°C) are independently associated with a higher mortality rate after severe TBI. The results suggest that, contrary to current opinion, temperatures within the normal to moderate fever range during the acute post-TBI period do not impose an additional risk for a poor outcome after severe TBI.
The effect of spontaneous alterations in brain temperature on outcome: a prospective observational cohort study in patients with severe traumatic brain injury.
J Neurotrauma. 2010 Dec;27(12):2157-64