The overall effect of the antifibrinolytic drug tranexamic acid on outcome from major trauma was assessed in the CRASH-2 trial, reported here and here. Its effect on a nested cohort of 270 patients from the trial who had traumatic brain injury has now been published1.
Previous evaluation in nontraumatic subarachnoid haemorrhage patients showed tranexamic acid to be associated with cerebral ischaemia, whereas in CRASH-2 (in which a lower dose of tranexamic acid was used) there was a trend to fewer ischaemic lesions as well as smaller haematoma growth and decreased mortality. None of these outcomes were statistically significant so further research is warranted.
An accompanying editorial2 states:
…the CRASH-2 study also justifies a re-evaluation of the possible benefit of low dose short term TXA in patients with other types of intracranial haemorrhage. Many patients with aneurysmal subarachnoid haemorrhage still have to wait for one or two days before the aneurysm is occluded. In addition, at least 30% of patients with spontaneous intracerebral haemorrhage experience substantial haematoma growth in the first 24 hours after the onset of the haemorrhage. As well as the CRASH-2 trial we therefore need new trials investigating short course low dose TXA in patients with aneurysmal subarachnoid haemorrhage and intracerebral haemorrhage.
It looks like considerable enthusiasm for this drug will be around for a while. I look forward to more outcome data, particularly in regard to this challenging group of patients with traumatic and non-traumatic intracranial bleeding.
OBJECTIVE: To assess the effect of tranexamic acid (which reduces bleeding in surgical patients and reduces mortality due to bleeding in trauma patients) on intracranial haemorrhage in patients with traumatic brain injury.
METHODS: A nested, randomised, placebo controlled trial. All investigators were masked to treatment allocation. All analyses were by intention to treat. Patients 270 adult trauma patients with, or at risk of, significant extracranial bleeding within 8 hours of injury, who also had traumatic brain injury.
INTERVENTIONS: Patients randomly allocated to tranexamic acid (loading dose 1 g over 10 minutes, then infusion of 1 g over 8 hours) or matching placebo.
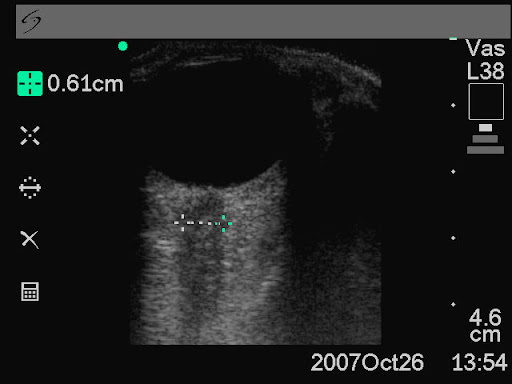
MAIN OUTCOME MEASURES: Intracranial haemorrhage growth (measured by computed tomography) between hospital admission and then 24-48 hours later, with adjustment for Glasgow coma score, age, time from injury to the scans, and initial haemorrhage volume.
RESULTS: Of the 133 patients allocated to tranexamic acid and 137 allocated to placebo, 123 (92%) and 126 (92%) respectively provided information on the primary outcome. All patients provided information on clinical outcomes. The mean total haemorrhage growth was 5.9 ml (SD 26.8) and 8.1 mL (SD 29.2) in the tranexamic acid and placebo groups respectively (adjusted difference -3.8 mL (95% confidence interval -11.5 to 3.9)). New focal cerebral ischaemic lesions occurred in 6 (5%) patients in the tranexamic acid group versus 12 (9%) in the placebo group (adjusted odds ratio 0.51 (95% confidence interval 0.18 to 1.44)). There were 14 (11%) deaths in the tranexamic acid group and 24 (18%) in the placebo group (adjusted odds ratio 0.47 (0.21 to 1.04)).
CONCLUSIONS: This trial shows that neither moderate benefits nor moderate harmful effects of tranexamic acid in patients with traumatic brain injury can be excluded. However, the analysis provides grounds for further clinical trials evaluating the effect of tranexamic acid in this population
1. Effect of tranexamic acid in traumatic brain injury: a nested randomised, placebo controlled trial (CRASH-2 Intracranial Bleeding Study)
BMJ. 2011 Jul 1;343:d379 (free text available)
2. Tranexamic acid for traumatic brain injury
BMJ. 2011 Jul 1;343:d3958