Body temperature raises heart rate and respiratory rate in kids, potentially affecting our interpretation of these clinical signs.
Dutch investigators developed centile charts of respiratory rates for specific body temperatures (derivation study), so that abnormally high rates could be identified as a means of predicting lower respiratory infection (validation set).
Respiratory rate increased overall by 2.2 breaths/min per 1°C rise (standard error 0.2) after accounting for age and temperature in the model, which is similar to a previous UK study that suggested a rise in respiratory rate of around 0.5-2 breaths per minute and an increase in heart rate of about 10 beats per minute for every 1 degree celcius above normal.
Cut-off values at the 97th centile were more useful in detecting the presence of LRTI than existing (Advanced Paediatric Life Support) respiratory rate thresholds.
The respiratory rate charts are available here.
Derivation and validation of age and temperature specific reference values and centile charts to predict lower respiratory tract infection in children with fever: prospective observational study
BMJ. 2012 Jul 3;345:e4224
Free Full Text Link
Tag Archives: pneumonia
Dexamethasone for community acquired pneumonia

Another Dutch study has examined steroids for community acquired pneumonia, this time with the primary outcome measure being hospital length of stay, which was reduced by one day on the steroid group. Compare this study with a previous negative study of prednisolone for pneumonia.
BACKGROUND: Whether addition of corticosteroids to antibiotic treatment benefits patients with community-acquired pneumonia who are not in intensive care units is unclear. We aimed to assess effect of addition of dexamethasone on length of stay in this group, which might result in earlier resolution of pneumonia through dampening of systemic inflammation.
METHODS: In our double-blind, placebo-controlled trial, we randomly assigned adults aged 18 years or older with confirmed community-acquired pneumonia who presented to emergency departments of two teaching hospitals in the Netherlands to receive intravenous dexamethasone (5 mg once a day) or placebo for 4 days from admission. Patients were ineligible if they were immunocompromised, needed immediate transfer to an intensive-care unit, or were already receiving corticosteroids or immunosuppressive drugs. We randomly allocated patients on a one-to-one basis to treatment groups with a computerised randomisation allocation sequence in blocks of 20. The primary outcome was length of hospital stay in all enrolled patients. This study is registered with ClinicalTrials.gov, number NCT00471640.
FINDINGS: Between November, 2007, and September, 2010, we enrolled 304 patients and randomly allocated 153 to the placebo group and 151 to the dexamethasone group. 143 (47%) of 304 enrolled patients had pneumonia of pneumonia severity index class 4-5 (79 [52%] patients in the dexamethasone group and 64 [42%] controls). Median length of stay was 6·5 days (IQR 5·0-9·0) in the dexamethasone group compared with 7·5 days (5·3-11·5) in the placebo group (95% CI of difference in medians 0-2 days; p=0·0480). In-hospital mortality and severe adverse events were infrequent and rates did not differ between groups, although 67 (44%) of 151 patients in the dexamethasone group had hyperglycaemia compared with 35 (23%) of 153 controls (p<0·0001).
INTERPRETATION: Dexamethasone can reduce length of hospital stay when added to antibiotic treatment in non-immunocompromised patients with community-acquired pneumonia.
Dexamethasone and length of hospital stay in patients with community-acquired pneumonia: a randomised, double-blind, placebo-controlled trial
Lancet. 2011 Jun 11;377(9782):2023-30
Steroids for trauma
 A French study on adult patients intubated for multiple trauma assessed the effect of a one week course of stress-dose hydrocortisone therapy against placebo on the incidence of hospital-acquired pneumonia. Multiple trauma was defined as having 2 or more traumatic injuries and an injury severity score higher than 15. The primary outcome measure was hospital-acquired pneumonia, defined by robust criteria and requiring positive lower respiratory tract microbiology. The study was not powered to detect a difference in mortality. The authors conclude that a stress dose of hydrocortisone for 7 days is associated with a reduction in the rate of hospital-acquired pneumonia at day 28 together with a decreased requirement for mechanical ventilation and length of ICU stay in trauma patients.
A French study on adult patients intubated for multiple trauma assessed the effect of a one week course of stress-dose hydrocortisone therapy against placebo on the incidence of hospital-acquired pneumonia. Multiple trauma was defined as having 2 or more traumatic injuries and an injury severity score higher than 15. The primary outcome measure was hospital-acquired pneumonia, defined by robust criteria and requiring positive lower respiratory tract microbiology. The study was not powered to detect a difference in mortality. The authors conclude that a stress dose of hydrocortisone for 7 days is associated with a reduction in the rate of hospital-acquired pneumonia at day 28 together with a decreased requirement for mechanical ventilation and length of ICU stay in trauma patients.
An accompanying editorial, highlighting the contrast in these results with those of other steroid-studies such as the CRASH trial, which used higher doses of steroid for a shorter period, cautions:
“the overall evidence suggests that further study with a larger sample size is needed to better define the safety profile and risk of mortality in this patient population.”
Context The role of stress-dose hydrocortisone in the management of trauma patients is currently unknown.
Objective To test the efficacy of hydrocortisone therapy in trauma patients.
Design, Setting, and Patients Multicenter, randomized, double-blind, placebo-controlled HYPOLYTE (Hydrocortisone Polytraumatise) study. From November 2006 to August 2009, 150 patients with severe trauma were included in 7 intensive care units in France.
Intervention Patients were randomly assigned to a continuous intravenous infusion of either hydrocortisone (200 mg/d for 5 days, followed by 100 mg on day 6 and 50 mg on day 7) or placebo. The treatment was stopped if patients had an appropriate adrenal response.
Main Outcome Measure Hospital-acquired pneumonia within 28 days. Secondary outcomes included the duration of mechanical ventilation, hyponatremia, and death.
Results One patient withdrew consent. An intention-to-treat (ITT) analysis included the 149 patients, a modified ITT analysis included 113 patients with corticosteroid insufficiency. In the ITT analysis, 26 of 73 patients (35.6%) treated with hydrocortisone and 39 of 76 patients (51.3%) receiving placebo developed hospital-acquired pneumonia by day 28 (hazard ratio [HR], 0.51; 95% confidence interval [CI], 0.30-0.83; P = .007). In the modified ITT analysis, 20 of 56 patients (35.7%) in the hydrocortisone group and 31 of 57 patients (54.4%) in the placebo group developed hospital-acquired pneumonia by day 28 (HR, 0.47; 95% CI, 0.25-0.86; P = .01). Mechanical ventilation–free days increased with hydrocortisone by 4 days (95% CI, 2-7; P = .001) in the ITT analysis and 6 days (95% CI, 2-11; P < .001) in the modified ITT analysis. Hyponatremia was observed in 7 of 76 (9.2%) in the placebo group vs none in the hydrocortisone group (absolute difference, −9%; 95% CI, −16% to −3%; P = .01). Four of 76 patients (5.3%) in the placebo group and 6 of 73 (8.2%) in the hydrocortisone group died (absolute difference, 3%; 95% CI, −5% to 11%; P = .44).
Conclusion In intubated trauma patients, the use of an intravenous stress-dose of hydrocortisone, compared with placebo, resulted in a decreased risk of hospital-acquired pneumonia.
Hydrocortisone therapy for patients with multiple trauma: the randomized controlled HYPOLYTE study
JAMA. 2011 Mar 23;305(12):1201-9
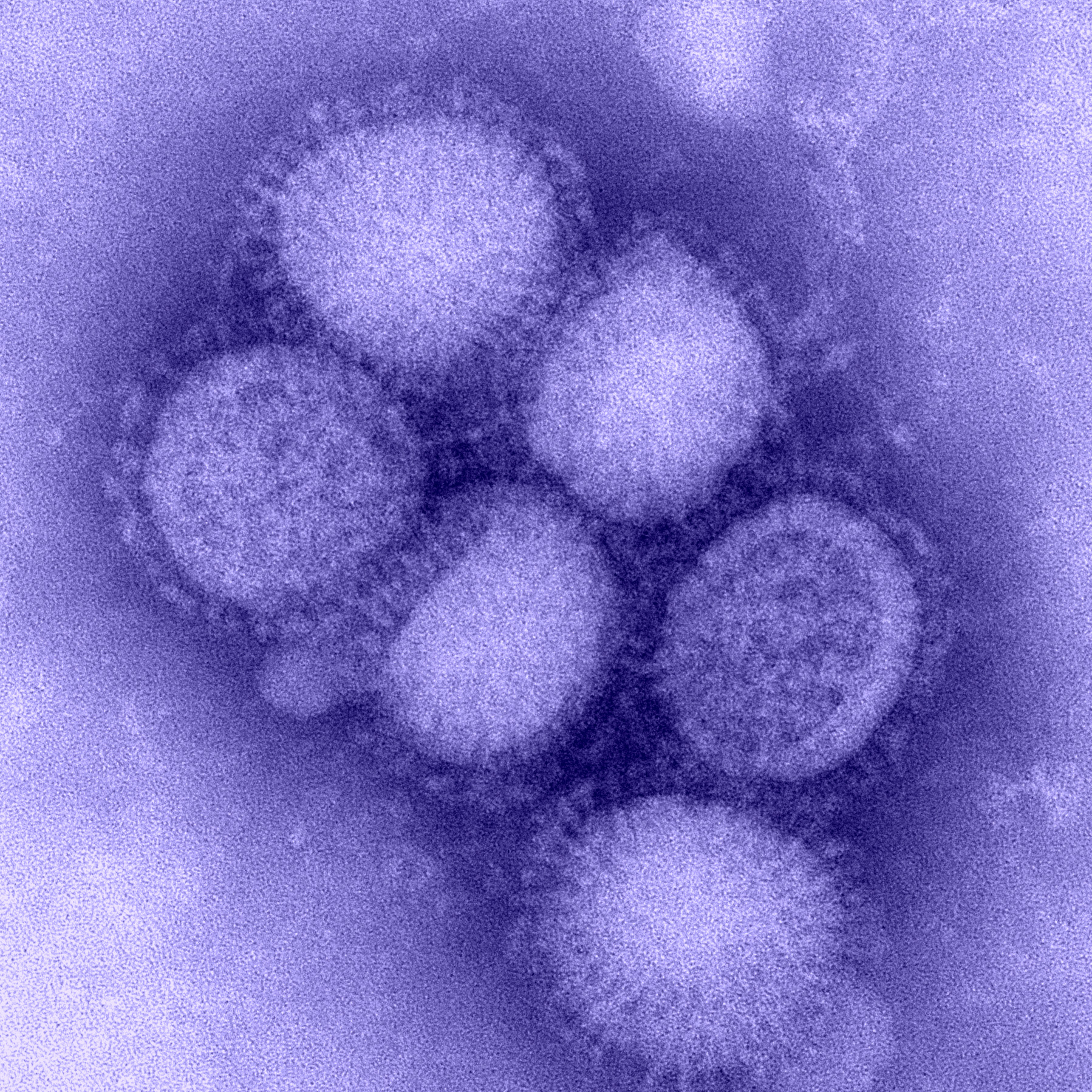
H1N1 or CAP?
A scoring system composed of clinical, radiological, and laboratory variables purports to distinguish H1N1 influenza virus infection from community acquired pneumonia1. An accompanying editorial2 suggests that while further validation is required, the most useful application of the score might be in those with a score of 0 or 1 (out of 5), in whom the the high negative predictive value might safely avoid inpatient isolation and neuraminidase inhibitor treatment in the under-65s.
Background Early identification of patients with H1N1 influenza-related pneumonia is desirable for the early instigation of antiviral agents. A study was undertaken to investigate whether adults admitted to hospital with H1N1 influenza-related pneumonia could be distinguished clinically from patients with non-H1N1 community-acquired pneumonia (CAP).
Methods Between May 2009 and January 2010, clinical and epidemiological data of patients with confirmed H1N1 influenza infection admitted to 75 hospitals in the UK were collected by the Influenza Clinical Information Network (FLU-CIN). Adults with H1N1 influenza-related pneumonia were identified and compared with a prospective study cohort of adults with CAP hospitalised between September 2008 and June 2010, excluding those admitted during the period of the pandemic.
Results Of 1046 adults with confirmed H1N1 influenza infection in the FLU-CIN cohort, 254 (25%) had H1N1 influenza-related pneumonia on admission to hospital. In-hospital mortality of these patients was 11.4% compared with 14.0% in patients with inter-pandemic CAP (n=648). A multivariate logistic regression model was generated by assigning one point for each of five clinical criteria: age ≤65 years, mental orientation, temperature ≥38°C, leucocyte count ≤12×10(9)/l and bilateral radiographic consolidation. A score of 4 or 5 predicted H1N1 influenza-related pneumonia with a positive likelihood ratio of 9.0. A score of 0 or 1 had a positive likelihood ratio of 75.7 for excluding it.
Conclusion There are substantial clinical differences between H1N1 influenza-related pneumonia and inter-pandemic CAP. A model based on five simple clinical criteria enables the early identification of adults admitted with H1N1 influenza-related pneumonia.
1. Clinical and laboratory features distinguishing pandemic H1N1 influenza-related pneumonia from interpandemic community-acquired pneumonia in adults
Thorax. 2011 March; 66(3): 247–252 Free Full Text
2. Predicting the unpredictable: is it possible clinically to separate H1N1 from non-H1N1 community-acquired pneumonia?
Thorax. 2011 Mar;66(3):187-8
Pneumonia scores equivalent
Got a favourite assessment tool for classifying the severity of community acquired pneumonia? Two systematic reviews showed no significant differences in performance between Pneumonia Severity Index (PSI) and various versions of CURB (CURB, CURB-65, and CRB-65).
An accompanying editorial* opines that CRB-65 is the simplest tool and can easily be remembered. It also discusses some of the more subtle strengths and weaknesses of the tools.
Severity assessment tools for predicting mortality in hospitalised patients with community-acquired pneumonia. Systematic review and meta-analysis
Thorax. 2010 Oct;65(10):878-83
Value of severity scales in predicting mortality from community-acquired pneumonia: systematic review and meta-analysis
Thorax. 2010 Oct;65(10):884-90
*Severity scores for CAP. ‘Much workload for the next bias’
Thorax 2010 Oct;65:853-855
Steroids for pneumonia?
Steroids are useful in asthma and COPD exacerbations, which are lung problems. Pneumonia is a lung infection, so steroids might help there too right? Erm… no.
A double blind randomised controlled trial demonstrated no benefit from steroids (prednisolone) versus placebo in patients with community acquired pneumonia, and late therapaeutic failure (>72 h after admission) was more common in the prednisolone group.
Efficacy of Corticosteroids in Community-acquired Pneumonia: A Randomized Double-Blinded Clinical Trial
Am J Respir Crit Care Med. 2010 May 1;181(9):975-82
ACEP pneumonia statement
The American College of Emergency Physicians has conducted an evidence review and issued a policy regarding two critical issues surrounding ED management of pneumonia: whether blood cultures should be taken and in what time frame antibiotics should be administered.
The full document is available from the ACEP website:
Clinical Policy: Critical Issues in the Management of Adult Patients Presenting to the Emergency Department With Community-Acquired Pneumonia