Dr Feynman talking about beauty is, well…beautiful
Monthly Archives: October 2011
Offensive medicine: CT before LP
I’m getting worn down by clinicians – often other specialists – who insist that CT imaging of the brain is mandatory prior to lumbar puncture in all patients. There is surely a subgroup of patients (especially young ones) in whom the benefit:harm balance of CT comes out in favour of NOT doing the imaging. In these cases, getting the scan is not ‘defensive medicine’ but ‘offensive medicine’ – offending the principle of primum non nocere. During ED shifts I have recently had to perform online searches in order to furnish colleagues and patients’ medically qualified relatives with printouts of the literature on this. This page is here to save me having to repeat those searches. Regarding the practice of performing a routine head CT prior to lumbar puncture to rule out risk of herniation:
- Mass effect on CT does not predict herniation
- Lack of mass effect on CT does not rule out raised ICP or herniation
- Herniation has occurred in patients who did not undergoing lumbar puncture because of CT findings
- Clinical predictors of raised ICP are more reliable than CT findings
- CT may delay diagnosis and treatment of meningitis
- Even in patients in whom LP may be considered contraindicated (cerebral abscess, mass effect on CT), complications from LP were rare in several studies
Best practice, it would seem, is the following
- If you think CT will show a cause for the headache, do a CT
- If a CT is indicated for other reasons (depressed conscious level, focal neurology), do a CT
- If a GCS 15 patient is to undergo LP for suspected (or to rule out) meningitis, and they have a normal neurological exam (including fundi), and are not elderly or immunosuppressed, there is no need to do a CT first.
- If you’re seriously worried about meningitis and are intent on getting a CT prior to LP, don’t let the imaging delay antimicrobial therapy.
Here are some useful references:
1. The CT doesn’t help
CT head before lumbar puncture in suspected meningitis BestBET evidence summary: In cases of suspected meningitis it is very unlikely that patients without clinical risk factors (immunocompromise/ history of CNS disease/seizures) or positive neurological findings will have a contraindication to lumbar puncture on their CT scan If CT scan is deemed to be necessary, administration of antibiotics should not be delayed. BestBETS website
Computed Tomography of the Head before Lumbar Puncture in Adults with Suspected Meningitis Much cited NEJM paper from 2001 which concludes: “In adults with suspected meningitis, clinical features can be used to identify those who are unlikely to have abnormal findings on CT of the head” N Engl J Med. 2001 Dec 13;345(24):1727-33 Full Text
Cranial CT before Lumbar Puncture in Suspected Meningitis Correspondence in 2002 NEJM including study of 75 patients with pneumococcal meningitis: CT cannot rule out risk of herniation Cranial CT before Lumbar Puncture in Suspected Meningitis N Engl J Med. 2002 Apr 18;346(16):1248-51 Full Text
2. The CT may harm
Cancer risk from CT Paucis verbis card, from the wonderful Academic Life in EM
3. Guidelines say CT is not always needed
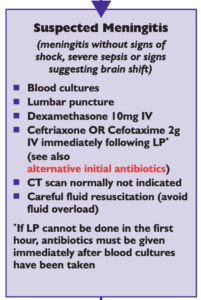
National (UK) guidelines on meningitis (community acquired meningitis in the immunocompetent host) available from meningitis.org. , including this box:
Practice Guidelines for the Management of Bacterial Meningitis These 2004 guidelines from the Infectious Diseases Society of America provide the following table listing the recommended criteria for adult patients with suspected bacterial meningitis who should undergo CT prior to lumbar puncture:
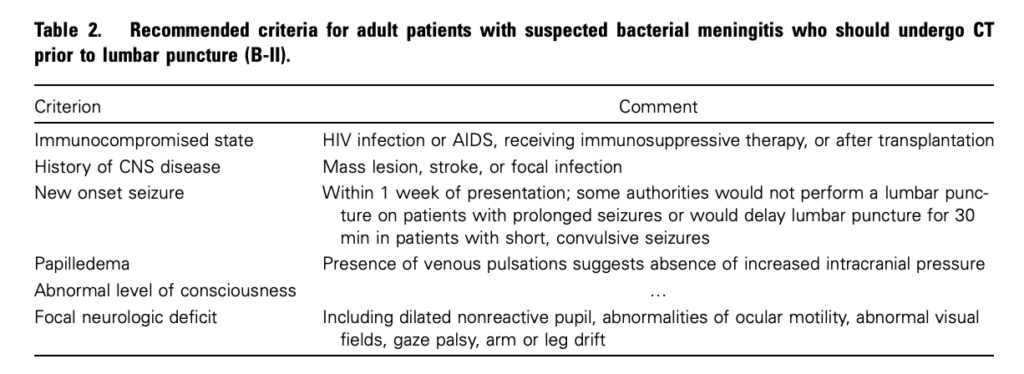
Clin Infect Dis. (2004) 39 (9): 1267-1284 Full text
4. This is potentially even more of an issue with paediatric patients
Fatal Lumbar Puncture: Fact Versus Fiction—An Approach to a Clinical Dilemma
An excellent summary of the above mentioned issues presented in a paediatric context, including the following:
On initial consideration a cranial CT would seem to be an appropriate and potentially useful diagnostic study for confirming the diagnosis of cerebral herniataion. The fallacy in this assessment has been emphasized by the finding that no clinically significant CT abnormalities are found that are not suspected on clinical assessments. Further, as previously noted, a normal CT examination may be found at about the time of a fatal herniation. Thus, the practical usefulness of a cranial CT in the majority of pediatric patients is limited to those rare patients whose increased ICP is secondary to mass lesions, not in the initial approach to acute meningitis.
Pediatrics. 2003 Sep;112(3 Pt 1):e174-6 Full Text
The last words should go to Dr Brad Spellberg, who in response to the IDSA’s guidelines wrote an excellent letter summarising much of the evidence at the time, confessed:
Why do we persist in using the CT scan for this purpose, despite the lack of supportive data? I am as guilty of this practice as anyone else, and the reason is simple: I am a chicken.
Salicylate poisoning and pseudohyperchloraemia

Severe salicylate poisoning can cause metabolic acidosis from an accumulation of salicylic acid, lactic acid, and ketone bodies. A high anion gap acidosis is therefore the typical metabolic abnormality seen. A case series illustrates salicylate poisoning presenting with a normal gap (hyperchloraemic) acidosis – one patient had a chloride of 111 mmol/l and the other 123 mmol/l. This can occur when some analysers falsely read an elevated chloride in the presence of high concentrations of salicylate.
Severe salicylate poisoning is classically associated with an anion gap metabolic acidosis. However, high serum salicylate levels can cause false increase of laboratory chloride results on some analyzers. We present 2 cases of life-threatening salicylate poisoning with an apparently normal anion gap caused by an important laboratory interference. These cases highlight that the diagnosis of severe salicylism must be considered in all patients presenting with metabolic acidosis, even in the absence of an increased anion gap.
Falsely Normal Anion Gap in Severe Salicylate Poisoning Caused by Laboratory Interference
Ann Emerg Med. 2011 Sep;58(3):280-1
Oxygen prevented hypoxia. Yep.

Why wouldn’t you give oxygen prophylactically to someone undergoing procedural sedation? One argument is that this will delay the detection of respiratory depression since a pre-oxygenated patient can be hyponoeic/apnoeic for longer prior to desaturation. This is not an issue for those of us who use non-invasive capnography during sedation.
In this randomized trial of oxygen vs air during ED propofol procedural sedation there was less hypoxia when high-flow supplemental oxygen was added. The authors made the following observations:
- There was no difference between groups in the incidence of respiratory depression, confirming previous research that supplemental oxygen does not exacerbate respiratory depression
- 5 patients in the compressed air group developed hypoxia without preceding respiratory depression, so capnography cannot be completely relied on in this setting.
They summarise:
“…assuming that capnography is in place to monitor ventilatory function, our results strongly support the routine use of high-flow oxygen during ED propofol sedation”
STUDY OBJECTIVE: We determine whether high-flow oxygen reduces the incidence of hypoxia by 20% in adults receiving propofol for emergency department (ED) sedation compared with room air.
METHODS: We randomized adults to receive 100% oxygen or compressed air at 15 L/minute by nonrebreather mask for 5 minutes before and during propofol procedural sedation. We administered 1.0 mg/kg of propofol, followed by 0.5 mg/kg boluses until the patient was adequately sedated. Physicians and patients were blinded to the gas used. Hypoxia was defined a priori as an oxygen saturation less than 93%; respiratory depression was defined as an end tidal CO(2) greater than 50 mm Hg, a 10% absolute change from baseline, or loss of waveform.
RESULTS: We noted significantly less hypoxia in the 59 patients receiving high-flow oxygen compared with the 58 receiving compressed air (19% versus 41%; P=.007; difference 23%; 95% confidence interval 6% to 38%). Respiratory depression was similar between groups (51% versus 48%; difference 2%; 95% confidence interval -15% to 22%). We observed 2 adverse events in the high-flow group (1 hypotension, 1 bradycardia) and 2 in the compressed air group (1 assisted ventilation, 1 hypotension).
CONCLUSION: High-flow oxygen reduces the frequency of hypoxia during ED propofol sedation in adults.
The Utility of High-Flow Oxygen During Emergency Department Procedural Sedation and Analgesia With Propofol: A Randomized, Controlled Trial
Ann Emerg Med. 2011 Oct;58(4):360-364
