
A resuscitationist agonises. These words, expressed by Scott Weingart during a podcast we did together, ring true to all of us who strive to improve our practice. Driven by the passionate conviction that we should never lose a salvageable patient through imperfect care, we relive cases and re-run them through our mental simulators to identify areas for improvement.
In the search for actionable items though, we occasionally exit this process empty-handed. Something about a case felt wrong although ostensibly all the clinical interventions may have been appropriate. It is in these cases that it can be helpful to have a structure to aid analysis.
I, along with an international, interdisciplinary faculty of resuscitationists, have previously proposed an easily remembered system for optimising the clinical and non-technical components of resuscitation immediately before and during a patient encounter, dubbed the ‘Zero Point Survey’ (ZPS)(1), so called because first contact with a patient is rarely ‘Time Zero’ for a prehospital mission or hospital resuscitation case; there is invariably time for preparation of oneself, one’s team, and the environment (including equipment) prior to the primary survey and commencement of resuscitation. Following the assessment and management of STEP (self, team, environment & patient), the team should be regularly Updated on patient status and informed of the Priorities.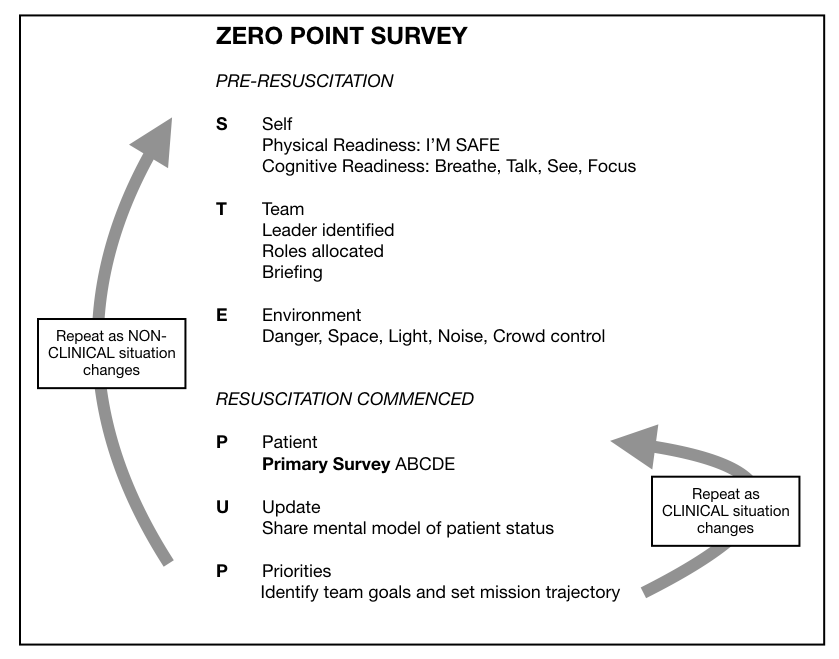
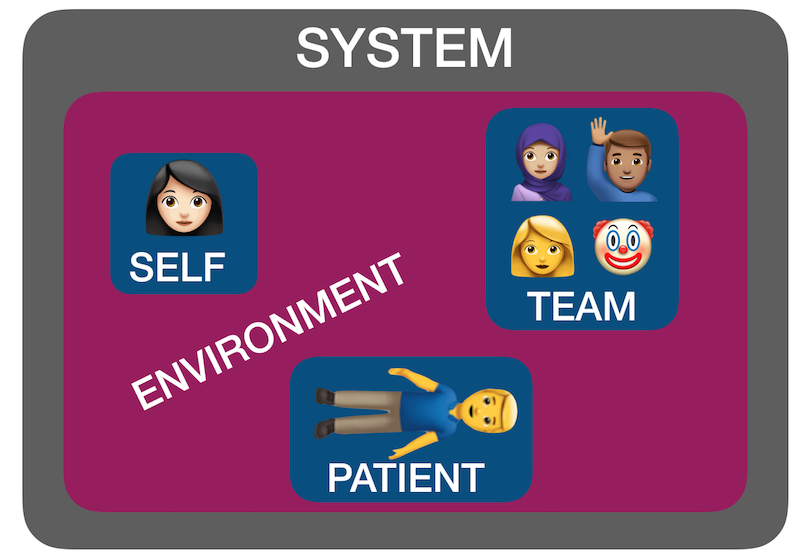
But ‘self, team, environment and patient’ isn’t just a useful system for case preparation. It can also be used for case analysis. I have found by discussing many ‘unsatisfactory’ cases over the years with participants in human factors workshops that STEP can help us identify where the issues lie. Accompanying all these factors is another ’S’: the system in which they interplay – the organisational rules, processes, policies, resources and deficiencies that may facilitate or obstruct an effective resuscitation(2).
Using STEPS to analyse cases
The following (genuinely) hypothetical resus cases demonstrate how the application of this framework – Self, Team, Environment, Patient, System – might help identify correctible factors for future resuscitations:
1. Cardiac arrest in the bathroom on the orthopaedic ward – “it was chaos, there were too many people, and the resus trolley wasn’t properly stocked”.
STEPS analysis:
Team – Leader needed to assign roles and allocate tasks
Environment – Crowd control needed, lack of equipment
System – Adequate checks for resus trolley not in place
2. 19-year-old male stabbed in the chest and arrested on arrival in hospital. CPR provided but went from PEA to asystole. Team leader discontinued resus after 20 minutes. Resident: “I thought he needed a resuscitative thoracotomy but no-one was willing to do it. No-one even mentioned it”.
STEPS analysis:
Self – Lacked confidence to speak up, doubted own knowledge or influence
Team – Lack of team situational awareness or knowledge or skill regarding required intervention
System – Insufficient training and preparation for penetrating traumatic cardiac arrest scenario
3. 30-year-old mother with abdominal wound and her 2-year-old daughter with massive open head injury, both due to gunshot wounds, having been shot by husband/father who killed himself on scene. Child arrests in the ED, without ROSC, witnessed by mother before mother is taken to operating theatre.
STEPS analysis:
Patient(s) – tragic case with upsetting circumstances and compounded psychological distress for patient and staff. The best resuscitation team in the world is not going to feel good about this one.
4. 46-year-old previously healthy male with VF arrest achieved ROSC after prehospital defibrillation and brought to the ED of a non-cardiac centre comatose and intubated. Further refractory VF in ED. Received multiple shocks, antiarrhythmics, double sequential external defibrillation. No on-site access to mechanical CPR, cardiac catheterisation, or ECMO. Patient declared dead in ED.
STEPS analysis:
System – Prehospital team gave excellent care but brought the patient to a hospital ill-equipped to manage his ongoing needs, due to lack of ambulance service policy regarding appropriate destination hospital for cardiac arrest cases.
Summary
You can see from the above cases how STEPS may be applied to make some sense of where a resus has gone wrong. Note that I am not recommending this as a way of structuring a team debrief or formal incident investigation – many institutions already have processes for conducting these and various rules and sensitivities have to be accommodated. Rather, this is a format I’ve found helpful in applying during informal discussions that aim to get the nub of where things could or should have gone better.
Occasionally, you can get a case where the STEPS seem to be aligned but things still feel bad – in which the outcome was unsatisfactory because the plan was wrong, or the team wasn’t able to execute the plan. In my next post I’ll discuss another way of analysing cases that can accompany STEPS.
1. Reid C, Brindley P, Hicks CM, Carley S, Richmond C, Lauria MJ, Weingart S. Zero point survey: a multidisciplinary idea to STEP UP resuscitation effectiveness. Clin Exp Emerg Med. 2018;5(3):139-143
2. Hicks C, Petrosoniak A. The Human Factor. Emergency Medicine Clinics of North America. 2018 Feb;36(1):1–17.
