Folks from the Medical University of Vienna have produced a great resource with free online echocardiography videos at www.123sonography.com
Check out their video on right heart endocarditis:
Category Archives: Ultrasound
Sonographic bits and bobs
Novel subclavian cannulation method
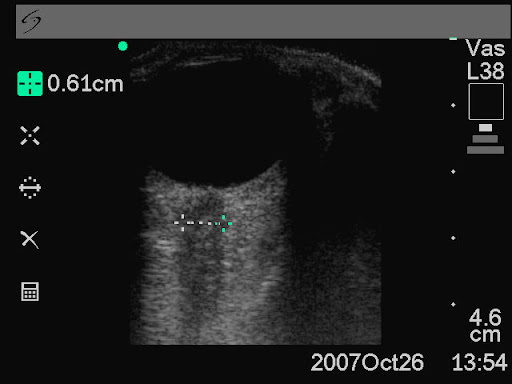
Ultrasound-guided subclavian vein cannulation has reduced complications, but there is still a high incidence of failure to cannulate the vein and of accidental arterial cannulation. Vassallo & Bennett noticed that a fast running intravenous infusion in the ipsilateral arm of a patient produced variable echogenicity (lighter echos) in the subclavian vein. They describe deliberately using this appearance to both identify the subclavian vein and differentiate it from the subclavian artery.
With the intravenous infusion running with frequent drips in the drip chamber, the ultrasound beam is placed in long axis to the subclavian vessels in the subclavicular position. The angle of the ultrasound beam is adjusted to reveal both the subclavian vein and artery. The variable echogenicity, together with compression, can then be used to identify the vein. The presence of variable echogenicity in the vessel gives continuous feedback that the ultrasound beam has not drifted onto the artery. In cases where the ultrasound beam has included both artery and vein in the same image, this method has clearly identified the intended target vessel.
Subclavian cannulation with ultrasound: a novel method
Anaesthesia, 2010;65:1041
Ultrasound measurement of optic nerve sheath diameter
Here’s the abstract from a new study contributing the literature on ED assessment of raised intracranial pressure using ocular ultrasound:
Background To assess if ultrasound measurement of the optic nerve sheath diameter (ONSD) can accurately predict the presence of raised intracranial pressure (ICP) and acute pathology in patients in the emergency department.
Methods This 3-month prospective observational study used ultrasound to measure the ONSD in adult patients who required CT from the emergency department. The mean ONSD from both eyes was measured using a 7.5 MHz ultrasound probe on closed eyelids. A mean ONSD value of >0.5 cm was taken as positive. Two radiologists independently assessed CT scans from patients in the study population for signs of raised ICP and signs of acute pathology (cerebrovascular accident, subarachnoid, subdural or extradural haemorrhage and tumour). Specificity, sensitivity and k values, for interobserver variability between reporting radiologists, were generated for the study data.
Results In all, 26 patients were enrolled into the study. The ONSD measurement was 100% specific (95% CI 79% to 100%) and 86% sensitive (95% CI 42% to 99%) for raised ICP. For any acute intracranial abnormality the value of ONSD was 100% specific (95% CI 76% to 100%) and 60% sensitive (95% CI 27% to 86%). k Values were 0.91 (95% CIs 0.73 to 1) for identification of raised ICP on CT and 0.84 (95% CIs 0.62 to 1) for any acute pathology on CT, between the radiologists.
Conclusions This study shows that ultrasound measurement of ONSD is sensitive and specific for raised ICP in the emergency department. Further observational studies are needed but this emerging technique could be used to focus treatment in unstable patients.
Ultrasound measurement of optic nerve sheath diameter in patients with a clinical suspicion of raised intracranial pressure
Emerg Med J. 2010 Aug 15. [Epub ahead of print]
Small bowel obstruction
When assessed against CT as gold standard, ultrasound diagnosis of small bowel obstruction by emergency physicians compared favourably with abdominal radiographs.

US exams were performed using a phased array probe in the bilateral colic gutters, epigastric and suprapubic regions to assess for (1) the presence of fluid-filled, dilated bowel (defined as >25mm) proximal to normal or collapsed bowel, and (2) decreased or absent bowel peristalsis (defined as back and forth movements of spot echoes inside the fluid-filled bowel). Either finding was considered ‘positive’ for small bowel obstruction.
Bedside ultrasonography for the detection of small bowel obstruction in the emergency department
Emerg Med J. 2010 Aug 22. [Epub ahead of print]
Asian Emergency Ultrasound Network
Got an interesting ultrasound case to share? You can upload it to the Asian Emergency Ultrasound Network. A great growing site run by Dr Mok Ka Leung in Hong Kong – a leading light in emergency medicine ultrasound in Asia.

http://www.aeun.org
Echo in life support feasible
Emergency physicians in Cambridge and Ipswich in the UK prospectively documented their echo use in cardiac arrest. Images were easily acquired, were quickly obtained, and influenced management. In keeping with previous studies, absence of ventricular wall motion predicted lack of return of spontaneous circulation, with a negative predictive value of 97%.

An evaluation of echo in life support (ELS): is it feasible? What does it add?
Emerg Med J. 2010 Oct 4. [Epub ahead of print]
McConnell's sign revisited
In acute pulmonary embolism, a well-recognised pattern of right ventricular wall motion reported by McConnell is characterised by normal RV apex (RVa) contractility with akinesia of the RV free wall. A study using an echo techique called longitudinal velocity vector imaging (VVI) was conducted to describe RVa mechanics in relation to the rest of the RV in patients with a proven acute PE (aPE) and to compare these results to healthy volunteers and to patients with known chronic pulmonary hypertension (cPH). There were no significant differences in segmental strain patterns between the aPE and cPH groups. The authors suggest that McConnell’s sign is probably a visual illusion; preserved RVa contractility might be due to tethering of the RVa to a hyperdynamic left ventricle in the presence of an acutely dilated RV and this is the most likely explanation of the regional pattern of RV dysfunction seen in aPE patients.
Video describing McConnell’s sign from YouTube:
Right Ventricular Apical Contractility in Acute Pulmonary Embolism: The McConnell Sign Revisited
Echocardiography. 2010 Jul;27(6):614-20
Pulmonary embolism echo
Academic Emergency Medicine has a free article on sonographic detection of submassive pumonary embolism, with three video clips.
One of the videos shows a nice demonstration of the McConnell sign (RV mid-segment dilation with apical sparing), which has been reported to be specific for (sub)massive PE. According to this article however, it has been reported that the McConnell sign is present in two thirds of patients with RV infarction and is only 33% specific for PE. Continuous wave Doppler helps differentiate RV infarction from submassive PE by demonstrating an increased tricuspid regurgitation RA-RV pressure gradient in submassive PE and a normal or low gradient in RV infarction.
The full article is available here
Another pneumoperitoneum
This Video from Academic Emergency Medicine shows distinct hyperechoic foci with reverberation artifacts visualised within free fluid, suggesting associated free intraperitoneal air (in a patient with a gastric perforation)
The full article is available here
Pneumoperitoneum
This video from the Trauma Association of Canada shows sonographic detection of intraperitoneal free air
[quicktime]http://www.traumacanada.org/media/pneumoperitoneum_video.mov[/quicktime]
