An observational cohort study of penetrating trauma patients treated by the Mobile Emergency Care Unit in Copenhagen, Denmark over a seven-and-a-half year period sought to determine the effect of on-scene time on 30-day mortality.
In this setting, in cases of penetrating trauma to the chest, or abdomen, a Mobile Emergency Care Unit (MECU) and Basic Life Support unit are dispatched simultaneously, and rendezvous at the site of the incident. The MECU is staffed with consultants in anaesthesiology, intensive care and emergency medicine, as well as a specially trained ALS provider.

The physician manning the MECU administers medication and is able to perform procedures such as intubation, thoracocentesis, pleural drainage, intravenous and intraosseous access for fluid resuscitation. Although some patients were in cardiac arrest due to penetrating torso trauma (9 patients received chest compressions, and all were dead at 30 follow up), thoracotomy was not listed as a skill provided.
Of the 467 patients registered, 442 (94.6%) were identified at the 30-day follow-up, of whom 40 (9%) were dead. A higher mortality was found among patients treated on-scene for more than 20 min (p<0.0001), although on-scene time was not a significant predictor of 30-day mortality in the multivariate analysis; OR 3.71, 95% CI 0.66 to 20.70 (p<0.14). The number of procedures was significantly correlated to a higher mortality in the multivariate analysis.
The authors conclude that on-scene time might be important in penetrating trauma, and ALS procedures should not delay transport to definite care at the hospital. However their adjusted Odds Ratio for on scene time >20 minutes as a predictor of 30 day mortality was 3.71 with very wide 95% confidence intervals (0.66 to 20.70) and there were several weaknesses and confounding factors in the study which the authors acknowledge.
The only real information this study provides appears to be on the idiosyncrasies of the Copenhagen pre-hospital care system. Looking at their list of procedures and their practice of chest compressions in cardiac arrest due to penetrating trauma, it is very hard to ascertain what, if any, advantage their physicians offer over trained paramedics. As the authors point out: “Currently, strict guidelines are not practiced. Hence, the decision to treat by a ‘scoop and run’ or a ‘stay and play’ approach is at the discretion of the physician”
On-scene time and outcome after penetrating trauma: an observational study
Emerg Med J. 2010 Oct 9. [Epub ahead of print]
Ultrasound measurement of optic nerve sheath diameter
Here’s the abstract from a new study contributing the literature on ED assessment of raised intracranial pressure using ocular ultrasound:
Background To assess if ultrasound measurement of the optic nerve sheath diameter (ONSD) can accurately predict the presence of raised intracranial pressure (ICP) and acute pathology in patients in the emergency department.
Methods This 3-month prospective observational study used ultrasound to measure the ONSD in adult patients who required CT from the emergency department. The mean ONSD from both eyes was measured using a 7.5 MHz ultrasound probe on closed eyelids. A mean ONSD value of >0.5 cm was taken as positive. Two radiologists independently assessed CT scans from patients in the study population for signs of raised ICP and signs of acute pathology (cerebrovascular accident, subarachnoid, subdural or extradural haemorrhage and tumour). Specificity, sensitivity and k values, for interobserver variability between reporting radiologists, were generated for the study data.
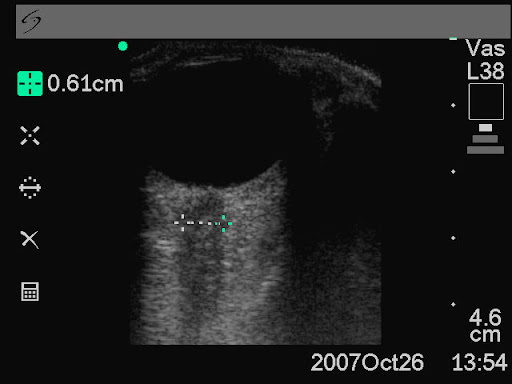
Results In all, 26 patients were enrolled into the study. The ONSD measurement was 100% specific (95% CI 79% to 100%) and 86% sensitive (95% CI 42% to 99%) for raised ICP. For any acute intracranial abnormality the value of ONSD was 100% specific (95% CI 76% to 100%) and 60% sensitive (95% CI 27% to 86%). k Values were 0.91 (95% CIs 0.73 to 1) for identification of raised ICP on CT and 0.84 (95% CIs 0.62 to 1) for any acute pathology on CT, between the radiologists.
Conclusions This study shows that ultrasound measurement of ONSD is sensitive and specific for raised ICP in the emergency department. Further observational studies are needed but this emerging technique could be used to focus treatment in unstable patients.
Ultrasound measurement of optic nerve sheath diameter in patients with a clinical suspicion of raised intracranial pressure
Emerg Med J. 2010 Aug 15. [Epub ahead of print]
Cirrhotic patients on ICU
The prognosis of cirrhotic patients with multiple organ failure is not universally dismal. A retrospective French study examined predictive factors of mortality and concluded: In-hospital survival rate of intensive care unit- admitted cirrhotic patients seemed acceptable, even in patients requiring life-sustaining treatments and/or with multiple organ failure on admission. The most important risk factor for in-hospital mortality was the severity of nonhematologic organ failure, as best assessed after 3 days. A trial of unrestricted intensive care for a few days could be proposed for select critically ill cirrhotic patients.
Cirrhotic patients in the medical intensive care unit: Early prognosis and long-term survival
Crit Care Med. 2010 Nov;38(11):2108-2116
Small bowel obstruction
When assessed against CT as gold standard, ultrasound diagnosis of small bowel obstruction by emergency physicians compared favourably with abdominal radiographs.

US exams were performed using a phased array probe in the bilateral colic gutters, epigastric and suprapubic regions to assess for (1) the presence of fluid-filled, dilated bowel (defined as >25mm) proximal to normal or collapsed bowel, and (2) decreased or absent bowel peristalsis (defined as back and forth movements of spot echoes inside the fluid-filled bowel). Either finding was considered ‘positive’ for small bowel obstruction.
Bedside ultrasonography for the detection of small bowel obstruction in the emergency department
Emerg Med J. 2010 Aug 22. [Epub ahead of print]
Pre-hospital RSI by different specialties
This aim of the study was to evaluate the tracheal intubation success rate of doctors drawn from different clinical specialities performing rapid sequence intubation (RSI) in the pre-hospital environment operating on the Warwickshire and Northamptonshire Air Ambulance. Over a 5-year period, RSI was performed in 200 cases (3.1/month).

Failure to intubate was declared if >2 successive attempts were required to achieve intubation or an ETT could not be placed correctly necessitating the use of an alternate airway. Successful intubation occurred in 194 cases, giving a failure rate of 3% (6 cases, 95% CI 0.6 to 5.3%). While no difference in failure rate was observed between emergency department (ED) staff and anaesthetists (2.73% (3/110, 95% CI 0 to 5.7%) vs 0% (0/55, 95% CI 0 to 0%); p=0.55), a significant difference was found when non-ED, non- anaesthetic staff (GP and surgical) were compared to anaesthetists (10.34% (3/29, 95% CI 0 to 21.4%) vs 0%; p=0.04). There was no significant difference associated with seniority of practitioner (p=0.65). The authors conclude that non-anaesthetic practitioners have a higher tracheal intubation failure rate during pre-hospital RSI, which may reflect a lack of training opportunities.
The small numbers of ‘failure’ rates, combined with the definition of failure in this study, make it hard to draw generalisations. Of note is that the paper lists the outcomes of the six patients who met the failed intubation definition, all of whom appear to have had their airway satisfactorily maintained by the RSI practitioner, three by eventual tracheal intubation, one by LMA, and two by surgical airway. More data are needed before whole specialties are judged on the performance of a small group of doctors.
Should non-anaesthetists perform pre-hospital rapid sequence induction? an observational study
Emerg Med J. 2010 Jul 26. [Epub ahead of print]
EM trainee RSI experience
A single centre observational study of rapid sequence intubation (RSI) was performed in a Scottish Emergency Department (ED) over four and a quarter years, followed by a postal survey of ED RSI operators.
There were 329 RSIs during the study period. RSI was performed by emergency physicians (both trained specialists and training grade, or ‘registrar’ doctors) in 288 (88%) patients. Complication rates were low and there were only two failed intubations requiring surgical airways (0.6%). ED registrars were the predominant RSI operator, with 206 patients (63%). ED consultants performed RSIs on 82 (25%) patients, anaesthetic registrars on 31 (9.4%) patients, and anaesthetic consultants on 8 (2.4%) patients. An ED consultant was present during every RSI performed and an anaesthetist was present during 72 (22%). The average number of ED registrars during this period of training was 8. This equates to each ED trainee performing approximately 26 ED RSIs (6.5 RSIs/year). On average, ED consultants performed 14 RSIs during this period (approx 3.5 RSIs/year). Of the 17 questionnaires, 12 were completed, in all of which cases the trainees were confident to perform RSI independently at the end of registrar training. Interestingly, 45 (14%) of the RSIs in the study were done in the pre-hospital environment by ED staff, two thirds of which were done by ED consultants.
Training and competency in rapid sequence intubation: the perspective from a Scottish teaching hospital emergency department
Emerg Med J. 2010 Sep 15. [Epub ahead of print]
Huge Solar Flare

NASA’s Solar Dynamics Observatory observed this ultraviolet image of one of the most intense solar flares witnessed in the past few months in sunspot 1112. A filament of magnetised material can be seen streaking 500,000 kilometres across the sun’s southern hemisphere. The bright spot just above the filament’s midpoint is UV radiation released from the sunspot. Read More from New Scientist
AED Use in Children Now Includes Infants
From the new 2010 resuscitation guidelines:
For attempted defibrillation of children 1 to 8 years of age with an AED, the rescuer should use a pediatric dose-attenuator system if one is available. If the rescuer provides CPR to a child in cardiac arrest and does not have an AED with a pediatric dose-attenuator system, the rescuer should use a standard AED. For infants (<1 year of age), a manual defibrillator is preferred. If a manual defibrillator is not available, an AED with pediatric dose attenuation is desirable. If neither is available, an AED without a dose attenuator may be used.

Summary: Adult AEDs may be used in all infants and children if there is no child-specific alternative
Highlights of the 2010 American Heart Association Guidelines for CPR and ECC
Cis-atracurium for ARDS
The ACURASYS study of atracurium vs placebo in ARDS: three ml rapid intravenous infusion of 15 mg of cis-atracurium besylate or placebo was administered, followed by a continuous infusion of 37.5 mg per hour for 48 hours. There appeared to be benefits in the intervention group, although the mechanisms are not clear. Further studies are needed.
BACKGROUND: In patients undergoing mechanical ventilation for the acute respiratory distress syndrome (ARDS), neuromuscular blocking agents may improve oxygenation and decrease ventilator-induced lung injury but may also cause muscle weakness. We evaluated clinical outcomes after 2 days of therapy with neuromuscular blocking agents in patients with early, severe ARDS.
METHODS: In this multicenter, double-blind trial, 340 patients presenting to the intensive care unit (ICU) with an onset of severe ARDS within the previous 48 hours were randomly assigned to receive, for 48 hours, either cisatracurium besylate (178 patients) or placebo (162 patients). Severe ARDS was defined as a ratio of the partial pressure of arterial oxygen (PaO2) to the fraction of inspired oxygen (FIO2) of less than 150, with a positive end-expiratory pressure of 5 cm or more of water and a tidal volume of 6 to 8 ml per kilogram of predicted body weight. The primary outcome was the proportion of patients who died either before hospital discharge or within 90 days after study enrollment (i.e., the 90-day in-hospital mortality rate), adjusted for predefined covariates and baseline differences between groups with the use of a Cox model.
RESULTS: The hazard ratio for death at 90 days in the cisatracurium group, as compared with the placebo group, was 0.68 (95% confidence interval [CI], 0.48 to 0.98; P=0.04), after adjustment for both the baseline PaO2:FIO2 and plateau pressure and the Simplified Acute Physiology II score. The crude 90-day mortality was 31.6% (95% CI, 25.2 to 38.8) in the cisatracurium group and 40.7% (95% CI, 33.5 to 48.4) in the placebo group (P=0.08). Mortality at 28 days was 23.7% (95% CI, 18.1 to 30.5) with cisatracurium and 33.3% (95% CI, 26.5 to 40.9) with placebo (P=0.05). The rate of ICU-acquired paresis did not differ significantly between the two groups.
CONCLUSIONS: In patients with severe ARDS, early administration of a neuromuscular blocking agent improved the adjusted 90-day survival and increased the time off the ventilator without increasing muscle weakness. (Funded by Assistance Publique-Hôpitaux de Marseille and the Programme Hospitalier de Recherche Clinique Régional 2004-26 of the French Ministry of Health; ClinicalTrials.gov number, NCT00299650.)
Neuromuscular blockers in early acute respiratory distress syndrome
N Engl J Med. 2010 Sep 16;363(12):1107-16

