Chest x-rays often miss pneumothoraces in the trauma room. These are occult pneumothoraces. A study using agreement by two fellowship trained radiologists as the gold standard for CXR interpretation showed that 80% of these were truly occult, ie. not detectable by the radiologists from CXR and only demonstrable on CT. Of those seven cases that could or should have been identified by emergency physicians (ie. ‘missed’ pneumothoraces) subcutaneous emphysema (5), pleural line (3), and deep sulcus sign (2) were detected by the radiologist reviewers.

This serves both as a reminder of the signs to look for on CXR for pneumothorax, and of the inadequacy of plain radiography in trauma patients. The authors advise in their discussion that ‘Thoracic ultrasonography may be the ideal diagnostic modality as it has a high sensitivity for the detection of PTX and it may be performed quickly at the bedside while maintaining spinal precautions’.
If you don’t know how to detect a pneumothorax with ultrasound yet, have a look here.
Occult Pneumothoraces Truly Occult or Simply Missed: Redux
J Trauma. 2010 Dec;69(6):1335-7
Tag Archives: Ultrasound
Great Ultrasound site
I recently had the pleasure of talking to some of the folks from the Henepin County Medical Centre Department of Emergency Medicine. What an inspiring group they are (they were the ones who wrote this article)!
They now have an awesome website at www.hqmeded.com with great ultrasound cases as well as other online lectures. Awesome.

ED US for DVT
Made a radiologist go red with rage recently? If not, you could try showing them this paper1 in this month’s Annals of Emergency Medicine that describes accurate emergency physician ultrasound diagnosis of deep vein thrombosis after just ten minutes training!
ED patients with a suspected lower extremity deep venous thrombosis were assessed using a bedside 2-point compression technique by emergency physicians using a portable US machine and all patients subsequently underwent duplex ultrasonography performed by the Department of Radiology.
The emergency physicians had a 10-minute training session before enrolling patients
The techinque involved 2 specific points: the common femoral and popliteal vessels, with subsequent compression of the common femoral and popliteal veins. The study result was considered positive for proximal lower extremity deep venous thrombosis if either vein was incompressible or a thrombus was visualised.

A total of 47 physicians performed 199 2-point compression ultrasonographic examinations in the ED.
There were 45 proximal lower extremity deep venous thromboses observed on Department of Radiology evaluation, all correctly identified by ED 2-point compression ultrasonography. The 153 patients without proximal lower extremity deep venous thrombosis all had a negative ED compression ultrasonographic result. One patient with a negative Department of Radiology ultrasonographic result was found to have decreased compression of the popliteal vein on ED compression ultrasonography, giving a single false-positive result, yet repeated ultrasonography by the Department of Radiology 1 week later showed a popliteal deep venous thrombosis. The sensitivity and specificity of ED 2-point compression ultrasonography for deep venous thrombosis were 100% (95% confidence interval 92% to 100%) and 99% (95% confidence interval 96% to 100%), respectively.
These figures may appear to fail the ‘sniff test’, ie. seem too good to be true. Not surprisingly Annals acknowledge this by providing an accompanying editorial2 by emergency ultrasound heavyweight Michael Blaivas, MD, who is healthily skeptical of such a minimal training program but is overwhelmingly supportive of the principle. Dr Blaivas also provides a fantastic summary of the existing evidence base on ED ultrasound for DVT. To me he hits the nail on the head when with a philosophical point on the practice of EM: ‘One common challenge proponents of any new application or procedure face in emergency medicine is overcoming the inertia of comfort with the status quo.’ Spot on, Dr B.
1. Compression Ultrasonography of the Lower Extremity With Portable Vascular Ultrasonography Can Accurately Detect Deep Venous Thrombosis in the Emergency Department
Annals of Emergency Medicine 2010;56(6):601-10
2. Point-of-Care Ultrasonographic Deep Venous Thrombosis Evaluation After Just Ten Minutes’ Training: Is This Offer Too Good to Be True?
Annals of Emergency Medicine 2010;56(6):611-3
The guys at ‘EM Live’ have a short video on how to do DVT ultrasound:
Aorta/IVC ratio and dehydration
Two studies this month report a correlation between ultrasound detected aorta/IVC ratio and dehydration in children presenting with diarrhoea and/or vomiting. In both studies the IVC diameter was measured in expiration and the aortic diameter in systole, using a transverse view in the subxiphoid area. Both used acute and post-discharge weight comparison to ascertain degree of dehydration.
The first study took place in Rwanda and a percent weight change between admission and discharge of greater than 10% was considered the criterion standard for severe dehydration. 52 children were included ranging in age from 1 month to 10 year. Vessel diameter measurements were inner wall to inner wall. The IVC-to-aorta ratio correlated significantly with percent weight change (r = 0.435, p < 0.001). Using the best ROC curve cutoff of 1.22, aorta/IVC ratio had a sensitivity of 93% (95% CI = 81% to 100%), specificity of 59% (95% CI = 44% to 75%), LR+ of 2.3 (95%CI=1.5to3.5), and LR– of 0.11 (95%CI=0.02to 0.76) for detecting severe dehydration. The same study did not find ultrasound assessment of inferior vena cava inspiratory collapse or the World Health Organization scale to be accurate predictors of severe dehydration in this same population of children.
Ultrasound Assessment of Severe Dehydration in Children With Diarrhea and Vomiting
Acad Emerg Med. 2010 Oct;17(10):1035-41
The second study took place in the USA. The subjects were considered to have significant dehydration if the weight loss was at least 5%. 71 were children were included. The area under the curve (AUC) was 0.73 (95% CI = 0.61 to 0.84). An IVC ⁄ aorta cutoff of 0.8 produced a sensitivity of 86% and a specificity of 56% for the diagnosis of significant dehydration. The positive predictive value was 56%, and the negative predictive value was 86%. Note this equates to an aorta/IVC ratio of 1.25, similar to that in the first study.
My rough-and-ready take home message from these two studies appears to be that an aorta/IVC ratio less than about 1.2 makes severe dehydration less likely in children with symptoms of gastroenteritis.
Use of Bedside Ultrasound to Assess Degree of Dehydration in Children With Gastroenteritis
Acad Emerg Med. 2010 Oct;17(10):1042-7
The Heart Point Sign
A case report describes the echo findings of a patient with a traumatic left sided pneumothorax. Although the subcostal view was unremarkable, upon imaging the parasternal region, the sonographer noted a flickering phenomenon where the heart was clearly visualized in late diastole, but would disappear in mid- systole only to reappear in late diastole during the next cardiac cycle. This ‘‘heart point’’ sign occurs because as the heart fills with blood in diastole, it enlarges and displaces the air from the precardiac space, allowing the heart to transiently contact the chest wall and be visualized with US. As the heart contracts during systole, the pneumothorax fills the space between the heart and the anterior chest wall, preventing the transmission of US and causing the heart to momentarily disappear from view.
The Heart Point Sign: Description of a New Ultrasound Finding Suggesting Pneumothorax
Academic Emergency Medicine 2010;17(11):e149–e150
Novel subclavian cannulation method
Ultrasound-guided subclavian vein cannulation has reduced complications, but there is still a high incidence of failure to cannulate the vein and of accidental arterial cannulation. Vassallo & Bennett noticed that a fast running intravenous infusion in the ipsilateral arm of a patient produced variable echogenicity (lighter echos) in the subclavian vein. They describe deliberately using this appearance to both identify the subclavian vein and differentiate it from the subclavian artery.
With the intravenous infusion running with frequent drips in the drip chamber, the ultrasound beam is placed in long axis to the subclavian vessels in the subclavicular position. The angle of the ultrasound beam is adjusted to reveal both the subclavian vein and artery. The variable echogenicity, together with compression, can then be used to identify the vein. The presence of variable echogenicity in the vessel gives continuous feedback that the ultrasound beam has not drifted onto the artery. In cases where the ultrasound beam has included both artery and vein in the same image, this method has clearly identified the intended target vessel.
Subclavian cannulation with ultrasound: a novel method
Anaesthesia, 2010;65:1041
Ultrasound measurement of optic nerve sheath diameter
Here’s the abstract from a new study contributing the literature on ED assessment of raised intracranial pressure using ocular ultrasound:
Background To assess if ultrasound measurement of the optic nerve sheath diameter (ONSD) can accurately predict the presence of raised intracranial pressure (ICP) and acute pathology in patients in the emergency department.
Methods This 3-month prospective observational study used ultrasound to measure the ONSD in adult patients who required CT from the emergency department. The mean ONSD from both eyes was measured using a 7.5 MHz ultrasound probe on closed eyelids. A mean ONSD value of >0.5 cm was taken as positive. Two radiologists independently assessed CT scans from patients in the study population for signs of raised ICP and signs of acute pathology (cerebrovascular accident, subarachnoid, subdural or extradural haemorrhage and tumour). Specificity, sensitivity and k values, for interobserver variability between reporting radiologists, were generated for the study data.
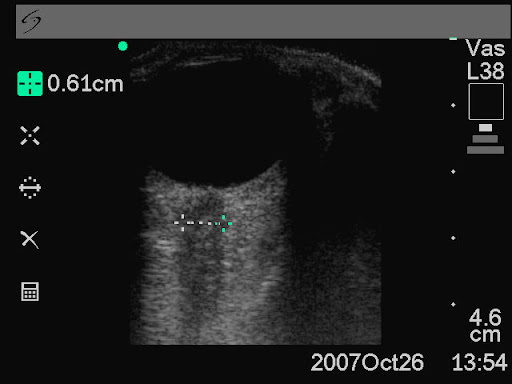
Results In all, 26 patients were enrolled into the study. The ONSD measurement was 100% specific (95% CI 79% to 100%) and 86% sensitive (95% CI 42% to 99%) for raised ICP. For any acute intracranial abnormality the value of ONSD was 100% specific (95% CI 76% to 100%) and 60% sensitive (95% CI 27% to 86%). k Values were 0.91 (95% CIs 0.73 to 1) for identification of raised ICP on CT and 0.84 (95% CIs 0.62 to 1) for any acute pathology on CT, between the radiologists.
Conclusions This study shows that ultrasound measurement of ONSD is sensitive and specific for raised ICP in the emergency department. Further observational studies are needed but this emerging technique could be used to focus treatment in unstable patients.
Ultrasound measurement of optic nerve sheath diameter in patients with a clinical suspicion of raised intracranial pressure
Emerg Med J. 2010 Aug 15. [Epub ahead of print]
Small bowel obstruction
When assessed against CT as gold standard, ultrasound diagnosis of small bowel obstruction by emergency physicians compared favourably with abdominal radiographs.

US exams were performed using a phased array probe in the bilateral colic gutters, epigastric and suprapubic regions to assess for (1) the presence of fluid-filled, dilated bowel (defined as >25mm) proximal to normal or collapsed bowel, and (2) decreased or absent bowel peristalsis (defined as back and forth movements of spot echoes inside the fluid-filled bowel). Either finding was considered ‘positive’ for small bowel obstruction.
Bedside ultrasonography for the detection of small bowel obstruction in the emergency department
Emerg Med J. 2010 Aug 22. [Epub ahead of print]
Echo in life support feasible
Emergency physicians in Cambridge and Ipswich in the UK prospectively documented their echo use in cardiac arrest. Images were easily acquired, were quickly obtained, and influenced management. In keeping with previous studies, absence of ventricular wall motion predicted lack of return of spontaneous circulation, with a negative predictive value of 97%.

An evaluation of echo in life support (ELS): is it feasible? What does it add?
Emerg Med J. 2010 Oct 4. [Epub ahead of print]
Another pneumoperitoneum
This Video from Academic Emergency Medicine shows distinct hyperechoic foci with reverberation artifacts visualised within free fluid, suggesting associated free intraperitoneal air (in a patient with a gastric perforation)
The full article is available here
