ECG machines may give a printed report saying ***ACUTE MI***. In a retrospective study, patients on the ICU whose 12 lead ECGs contained this electronic interpretation did not have an elevated troponin 85% of the time. Even in the minority of patients whose electronic ECG diagnosis of MI was agreed with by a cardiologist, only one third developed an elevated troponin.
The authors state ‘In contrast to nonintensive care unit patients who present with chest pain, the electrocardiographic ST-segment elevation myocardial infarction diagnosis seems to be a nonspecific finding in the intensive care unit that is frequently the result of a variety of nonischaemic processes. The vast majority of such patients do not have frank ST-segment elevation myocardial infarction.’
Electrocardiographic ST-segment elevation myocardial infarction in critically ill patients: An observational cohort analysis
Crit Care Med. 2010 Dec;38(12):2304-230
Category Archives: Acute Med
Acute care of the medically sick adult
The Heart Point Sign
A case report describes the echo findings of a patient with a traumatic left sided pneumothorax. Although the subcostal view was unremarkable, upon imaging the parasternal region, the sonographer noted a flickering phenomenon where the heart was clearly visualized in late diastole, but would disappear in mid- systole only to reappear in late diastole during the next cardiac cycle. This ‘‘heart point’’ sign occurs because as the heart fills with blood in diastole, it enlarges and displaces the air from the precardiac space, allowing the heart to transiently contact the chest wall and be visualized with US. As the heart contracts during systole, the pneumothorax fills the space between the heart and the anterior chest wall, preventing the transmission of US and causing the heart to momentarily disappear from view.
The Heart Point Sign: Description of a New Ultrasound Finding Suggesting Pneumothorax
Academic Emergency Medicine 2010;17(11):e149–e150
Venous gas in COPD exacerbation
Prolific emergency medicine researcher Anne-Maree Kelly and colleague Dr Lim from Tan Tock Seng Hospital in Singapore have published a systematic review of articles assessing the utility of peripheral venous blood gases (pVBG) in exacerbations of COPD1. Their conclusion:
Available evidence suggests that there is good agreement for pH and HCO3 values between arterial and pVBG results in patients with COPD, but not for pO2 or pCO2. Widespread clinical use is limited because of the lack of validation studies on clinical outcomes
pVBG may however be useful as a screening test for significant arterial hypercarbia; Kelly et al. previously reported2 a cutoff value of 45 mmHg (5.9 kPa).
1. A meta-analysis on the utility of peripheral venous blood gas analyses in exacerbations of chronic obstructive pulmonary disease in the emergency department
Eur J Emerg Med. 2010 Oct;17(5):246-8
2. Kelly AM, Kerr D, Middleton P. Validation of venous pCO2 to screen for arterial hypercarbia in patients with chronic obstructive airways disease.
J Emerg Med 2005; 28:377–379
A-a gradient unhelpful in pregnancy
Given that thromboembolism is the leading cause of maternal death in the UK according to the latest UK CEMACE report, it would be nice to have reliable non-ionising tests in the ED to rapidly rule out this disease in pregnant women. Unfortunately, the alveolar-arterial oxygen gradient does not do the job.
A recent study compared the A-a gradient with CTPA as the gold standard. Of 102 patients who were pregnant or up to 6 weeks post-partum, there were 13 PEs (2 antepartum and 11 postpartum). The best sensitivity, specificity, and negative and positive predictive values for A-a gradients were 76.9%, 20.2%, 80.0%, and 11.5%, respectively.
Assessment of the alveolar-arterial oxygen gradient as a screening test for pulmonary embolism in pregnancy
Am J Obstet Gynecol. 2010 Oct;203(4):373.e1-4
CVCs placed in the ED
 Central lines in the ED are more likely to get infected because they’re inserted under less scrupulously aseptic conditions than in ICU, done more urgently, and are more likely to be placed in the mucky old femoral site by clumsy emergency physicians who don’t wash their hands after scratching their arses. Anyway, the intensivists will usually replace them with a ‘more ideal’ line after ICU admission. Right? Well, that’s what’s often taught and assumed to be the case, but a new study from a single centre suggests otherwise. ED-placed central venous catheters (19% of which were femoral) were typically left in for 4 to 5 days. The infection rate was 1.9 per 1,000 catheter-days, similar to that reported for central lines in other ICU case series.
Central lines in the ED are more likely to get infected because they’re inserted under less scrupulously aseptic conditions than in ICU, done more urgently, and are more likely to be placed in the mucky old femoral site by clumsy emergency physicians who don’t wash their hands after scratching their arses. Anyway, the intensivists will usually replace them with a ‘more ideal’ line after ICU admission. Right? Well, that’s what’s often taught and assumed to be the case, but a new study from a single centre suggests otherwise. ED-placed central venous catheters (19% of which were femoral) were typically left in for 4 to 5 days. The infection rate was 1.9 per 1,000 catheter-days, similar to that reported for central lines in other ICU case series.
Infection and Natural History of Emergency Department–Placed Central Venous Catheters
Annals of Emergency Medicine 2010;56(5):492-7
GPIIb/IIIa inhibitors
A systematic review on use of GPIIb/IIIa inhibitors in NSTEACS has been updated as part of the Annals of Emergency Medicine‘s Evidence Based Emergency Medicine series. The bottom line:
In patients with non-ST-segment elevation acute coronary syndromes who do not undergo early percutaneous coronary intervention, administration of platelet glycoprotein IIb/IIIa (GPIIb/IIIa) inhibitors, given in addition to aspirin and unfractionated heparin, does not reduce 30-day or 6-month mortality. For the composite endpoint of myocardial infarction or death, there was modest benefit at 30 days and 6 months; however, there was an increased risk of major hemorrhage among those receiving GPIIb/IIIa inhibitors.
Update: Use of Platelet Glycoprotein IIb/IIIa Inhibitors in Patients With Unstable Angina and Non-ST-Segment Elevation Myocardial Infarction
Annals of Emergency Medicine Volume 56, Issue 5 , Pages e1-e2, November 2010

Compare this with the recommendations of the European Resuscitation Council who provide the following summary regarding this class of drug:
Gp IIB/IIIA receptor inhibition is the common final link of platelet aggregation. Eptifibatide and tirofiban lead to reversible inhibition, while abciximab leads to irreversible inhibition of the Gp IIB/IIIA receptor. Older studies from the pre-stent era mostly support the use of this class of drugs. Newer studies mostly document neutral or worsened outcomes. Finally in most supporting, as well as neutral or opposing studies, bleeding occurred in more patients treated with Gp IIB/IIIA receptor blockers. There are insufficient data to support routine pre-treatment with Gp IIB/IIIA inhibitors in patients with STEMI or non-STEMI-ACS. For high-risk patients with non-STEMI-ACS, in-hospital upstream treatment with eptifibatide or tirofiban may be acceptable whereas abciximab may be given only in the context of PCI. Newer alternatives for antiplatelet treatment should be considered because of the increased bleeding risk with Gp IIB/IIIA inhibitors when used with heparins.
European Resuscitation Council Guidelines for Resuscitation 2010 Section 5. Initial management of acute coronary syndromes
Resuscitation 81 (2010) 1353–1363 – full text downloadable
High flow O2 and mortality in COPD
Titrated oxygen treatment significantly reduced mortality, hypercapnia, and respiratory acidosis compared with high flow oxygen in acute exacerbations of chronic obstructive pulmonary disease. The authors claim: ‘For high flow oxygen treatment in patients with confirmed chronic obstructive pulmonary disease in the prehospital setting, the number needed to harm was 14; that is, for every 14 patients who are given high flow oxygen, one will die.‘
The authors did not report data on the in-hospital management of the patients.
Effect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: randomised controlled trial
BMJ. 2010 Oct 18;341:c5462
Novel subclavian cannulation method
Ultrasound-guided subclavian vein cannulation has reduced complications, but there is still a high incidence of failure to cannulate the vein and of accidental arterial cannulation. Vassallo & Bennett noticed that a fast running intravenous infusion in the ipsilateral arm of a patient produced variable echogenicity (lighter echos) in the subclavian vein. They describe deliberately using this appearance to both identify the subclavian vein and differentiate it from the subclavian artery.
With the intravenous infusion running with frequent drips in the drip chamber, the ultrasound beam is placed in long axis to the subclavian vessels in the subclavicular position. The angle of the ultrasound beam is adjusted to reveal both the subclavian vein and artery. The variable echogenicity, together with compression, can then be used to identify the vein. The presence of variable echogenicity in the vessel gives continuous feedback that the ultrasound beam has not drifted onto the artery. In cases where the ultrasound beam has included both artery and vein in the same image, this method has clearly identified the intended target vessel.
Subclavian cannulation with ultrasound: a novel method
Anaesthesia, 2010;65:1041
Ultrasound measurement of optic nerve sheath diameter
Here’s the abstract from a new study contributing the literature on ED assessment of raised intracranial pressure using ocular ultrasound:
Background To assess if ultrasound measurement of the optic nerve sheath diameter (ONSD) can accurately predict the presence of raised intracranial pressure (ICP) and acute pathology in patients in the emergency department.
Methods This 3-month prospective observational study used ultrasound to measure the ONSD in adult patients who required CT from the emergency department. The mean ONSD from both eyes was measured using a 7.5 MHz ultrasound probe on closed eyelids. A mean ONSD value of >0.5 cm was taken as positive. Two radiologists independently assessed CT scans from patients in the study population for signs of raised ICP and signs of acute pathology (cerebrovascular accident, subarachnoid, subdural or extradural haemorrhage and tumour). Specificity, sensitivity and k values, for interobserver variability between reporting radiologists, were generated for the study data.
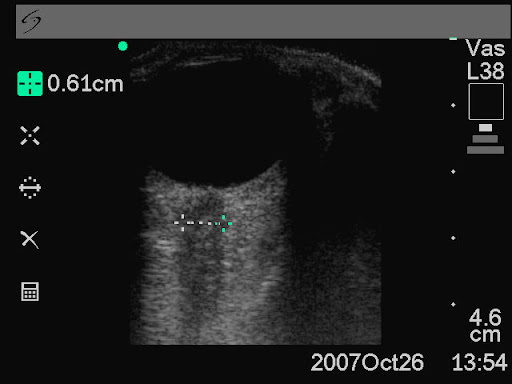
Results In all, 26 patients were enrolled into the study. The ONSD measurement was 100% specific (95% CI 79% to 100%) and 86% sensitive (95% CI 42% to 99%) for raised ICP. For any acute intracranial abnormality the value of ONSD was 100% specific (95% CI 76% to 100%) and 60% sensitive (95% CI 27% to 86%). k Values were 0.91 (95% CIs 0.73 to 1) for identification of raised ICP on CT and 0.84 (95% CIs 0.62 to 1) for any acute pathology on CT, between the radiologists.
Conclusions This study shows that ultrasound measurement of ONSD is sensitive and specific for raised ICP in the emergency department. Further observational studies are needed but this emerging technique could be used to focus treatment in unstable patients.
Ultrasound measurement of optic nerve sheath diameter in patients with a clinical suspicion of raised intracranial pressure
Emerg Med J. 2010 Aug 15. [Epub ahead of print]
Small bowel obstruction
When assessed against CT as gold standard, ultrasound diagnosis of small bowel obstruction by emergency physicians compared favourably with abdominal radiographs.

US exams were performed using a phased array probe in the bilateral colic gutters, epigastric and suprapubic regions to assess for (1) the presence of fluid-filled, dilated bowel (defined as >25mm) proximal to normal or collapsed bowel, and (2) decreased or absent bowel peristalsis (defined as back and forth movements of spot echoes inside the fluid-filled bowel). Either finding was considered ‘positive’ for small bowel obstruction.
Bedside ultrasonography for the detection of small bowel obstruction in the emergency department
Emerg Med J. 2010 Aug 22. [Epub ahead of print]
