A Japanese study of over 10,000 patients demonstrated improved neurological outcome in out-of-hospital cardiac arrest patients who were taken to hospitals designated as ‘critical care medical centres’, where neurologically favorable 1-month survival was greater [6.7% versus 2.8%, P < 0.001] despite a slightly longer call-hospital arrival interval [30.6 min vs 27.2, p < 0.001]. If return of spontaneous circulation was achieved pre-hospital, there was no difference in survival. It is unclear what factors, such as more interventional cardiology or therapeutic hypothermia, made the difference in the critical care centres.
Impact of transport to critical care medical centers on outcomes after
out-of-hospital cardiac arrest
Resuscitation. 2010 May;81(5):549-54
Category Archives: All Updates
Distance to hospital did not affect arrest survival
In a study of over 7500 patients with cardiac arrest transported by EMS in the United States, transport distance was not associated with survival on logistic analysis (OR 1.00; 95% CI 0.99–1.01).
A geospatial assessment of transport distance and survival to discharge in out of
hospital cardiac arrest patients: Implications for resuscitation centers
Resuscitation. 2010 May;81(5):518-23
Best position for CPR
A study using volunteer doctors and nurses in simulated cardiac arrest resuscitations compared three different positions for delivering CPR: standing, kneeling by the patient, or standing on a “taboret”. They measured rescuer fatigue and effectiveness of CPR. They conclude that CPR is best performed in a kneeling position in that it maximizes duration of effective chest compression and minimizes back pain. The authors recommend if two or more experienced healthcare providers are available to perform CPR, alternating rescuers every 2 min in the kneeling or standing on a taboret positions, and every 1min in the standing on the floor position in order to minimize rescuer fatigue.
Rescuer fatigue and cardiopulmonary resuscitation positions: A randomized controlled crossover trial
Resuscitation. 2010 May;81(5):579-84
Early CT and post-arrest outcome
A study on the early CT appearances of post-cardiac arrest patients shows two signs to be of importance – loss of boundary (LOB) between white and grey matter (at the level of the basal ganglia), and cortical sulcal effacement (SE). These features were more prevalent in patients who had > 20 minutes of arrest time and were associated with a worse neurological outcome at six months.
Early CT signs in out-of-hospital cardiac arrest survivors: Temporal profile and
prognostic significance
Resuscitation. 2010 May;81(5):534-8
Higher D Dimer cut-off in older patients
D-dimer levels below the conventional cut-off point of 500 µg/l combined with a “low/intermediate” or “unlikely” clinical probability can safely rule out the diagnosis in about 30% of patients with suspected pulmonary embolism.
However, the D-dimer concentration increases with age and its specificity for embolism decreases, which makes the test less useful to exclude pulmonary embolism in older patients; the test is able to rule out pulmonary embolism in 60% of patients aged <40 years, but in only 5% of patients aged >80.
A new, age dependent cut-off value was derived and then validated in two independent retrospective datasets from Belgium, France, the Netherlands, and Switzerland. They studied over 5000 patients aged >50 years.
The new D-dimer cut-off value was defined as (patient’s age x 10) µg/l in patients aged >50.
In 1331 patients in the derivation set with an “unlikely” score from clinical probability assessment, pulmonary embolism could be excluded in 42% with the new cut-off value versus 36% with the old cut-off value (<500 µg/l). In the two validation sets, the increase in the proportion of patients with a D-dimer below the new cut-off value compared with the old value was 5% and 6%. This absolute increase was largest among patients aged >70 years, ranging from 13% to 16% in the three datasets. The failure rates (all ages) were 0.2% (95% CI 0% to 1.0%) in the derivation set and 0.6% (0.3% to 1.3%) and 0.3% (0.1% to 1.1%) in the two validation sets.
Potential of an age adjusted D-dimer cut-off value to improve the exclusion of pulmonary embolism in older patients: a retrospective analysis of three large cohorts.
BMJ. 2010 Mar 30;340:c1475
TIA and stroke definitions
A quick reminder of the current defintions, as these have changed a couple of times over the last few years:
- Transient ischemic attack (TIA): a transient episode of neurological dysfunction caused by focal brain, spinal cord, or retinal ischemia, without acute infarction.
- An ischemic stroke is defined as an infarction of central nervous system tissue.
Definition and Evaluation of Transient Ischemic Attack: A Scientific Statement for Healthcare Professionals From the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease: The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists.
Stroke. 2009 Jun;40(6):2276-93 Full Text
STEMI and PCI guidelines
Lots of interesting and up to date information in this thick document from December 2009
Full text is available here
2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction (Updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (Updating the 2005 Guideline and 2007 Focused Update)
Protected: Positive capnography in cadavers
Thoracic Aortic Disease Guidelines
Guidelines for the Diagnosis and Management of Patients With Thoracic Aortic Disease have been published by a collaboration between a number of professional bodies including the American Heart Association.
Guidelines for the Diagnosis and Management of Patients With Thoracic Aortic Disease
Circulation. 2010 Apr 6;121(13):e266-369 – free Full Text as PDF
HTML full text
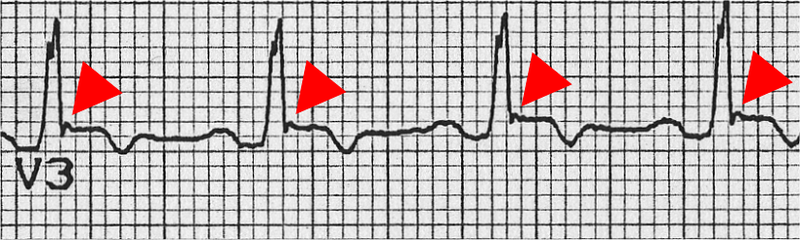
Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia
This disease may result in sudden cardiac death in young people, and the assessment of patients who present with dysrhythmias or syncope should prompt a review of the ECG for suggestive features of Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia (as well as ischaemia, conduction deficits, WPW syndrome, Brugada syndrome, and prolonged QT interval).
A Task force has revised its diagnostic criteria for the disease, listed as major and minor criteria pertaining to family history, ECG, echo, MRI, and angiographic features. The ECG features that front line doctors need to be on the look out for include:
- Inverted T waves in right precordial leads (V1, V2, and V3) or beyond in individual >14 years of age (in the absence of complete right bundle-branch block QR>120 ms)
- Inverted T waves in leads V1 and V2 in individual>14 years of age (in the absence of complete right bundle-branch block) or in V4, V5, or V6
- Inverted T waves in leads V1, V2, V3, and V4 in individual>14 years of age in the presence of complete right bundle-branch block
- Epsilon wave (reproducible low-amplitude signals between end of QRS complex to onset of the T wave) in the right precordial leads (V1 to V3)
- Nonsustained or sustained ventricular tachycardia of left bundle-branch morphology with superior axis (negative or indeterminate QRS in leads II, III, and aVF and positive in lead aVL)
- Nonsustained or sustained ventricular tachycardia of RV outflow configuration, left bundle-branch block morphology with inferior axis (positive QRS in leads II, III, and aVF and negative in lead aVL) or of unknown axis
- >500 ventricular extrasystoles per 24 hours (Holter)
Diagnosis of Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia Proposed Modification of the Task Force Criteria
Circulation. 2010 Apr 6;121(13):1533-41
More info on this disease from the European Society of Cardiology here
