Day three is Air Ambulance and pre-hospital day and the great and the good are here en mass.
The heavy weights are coming out to make their points…..
 Unarguably the best lecture of the day was delivered by our very own Cliff Reid on prehospital training. Using Sydney HEMS induction training he highlighted the challenges posed to prehospital services training doctors and paramedics rotating through the service.
Unarguably the best lecture of the day was delivered by our very own Cliff Reid on prehospital training. Using Sydney HEMS induction training he highlighted the challenges posed to prehospital services training doctors and paramedics rotating through the service.
Turning a good inhospital doctor into a great prehospital one in the space of an induction program requires focus. Knowledge is therefore not the focus of training, performance is. Often doctors already possess the clinical skills and knowledge and it is the application of these pre existing skills in challenging environments when cognitively overloaded that is the key.
The Sydney HEMS program provides the mindware and communication skills the practitioner needs to do this and drills these skills in simulated environments. He uses perturbation, so like the Bruce protocol exercise test the simulations just get harder until you are at the very limits of your bandwidth. Debriefing of course is important but the recommended protracted debrief is often impractical and unnecessary so simulations designed with cognitive traps are used to highlight learning points and are drilled until the message is received. In this way tress exposure enhances cognitive resilience. And importantly they use cross training, so the doctors and the paramedics undergo the same program so each member of the team understands the challenges faced by the other.
Does this sound like fun? For the shrinking violets out there it could be seen as threatening. But for the adrenaline junkies…….hell yeah!
It’s truly a training ethos that I buy into and I’d love to be able to achieve that standard of training in my own service.

 Microwaves seem to be the future if diagnostic testing. This modality is fast, is associated with a radiation dose lower than that of a mobile phone, non invasive, portable and has been shown to provide good information. It can be used on heads for intracranial haemorrhage and stroke or chests for pneumothorax detection. It’s all in the early stages but seems like it will be a viable option in the future.
Microwaves seem to be the future if diagnostic testing. This modality is fast, is associated with a radiation dose lower than that of a mobile phone, non invasive, portable and has been shown to provide good information. It can be used on heads for intracranial haemorrhage and stroke or chests for pneumothorax detection. It’s all in the early stages but seems like it will be a viable option in the future.
For further reading check out:
Diagnosis of subdural and intraparenchymal intracranial hemorrhage using a microwave-based detector
Clinical trial on subdural detection
Pneumothorax detection
How would you transfer a psychotic patient requiring specialist intervention that can only be received after aeromedical transfer? Stefan Mazur of MedSTAR, the retrieval service in South Australia shared their experience with ketamine to facilitate the safe transfer of these patients with no reports of adverse effects on the mental state of the patient, as first described by Minh Le Cong and colleagues. Is there no end to the usefulness of this drug? No wonder we’re experiencing a supply issue in the UK!
And finally, the ultimate reflective practice should include the post mortem of our critically sick patients. The approach the forensic pathologist takes is similar to a clinician (with the time pressure removed). They read the scene and use this information to predict injuries (sound familiar?). Post mortem CT scanning with recon provides yet another layer of information. We are missing a trick if we don’t seek this feedback to correlate with our clinical findings. Even better, rare practical skills are often routinely performed as part of the post mortem – we should be making use of this opportunity to train.
Tag Archives: imaging
Swallow a camera in GI bleed
Two recent studies evaluate the use of a novel ingestable camera to diagnose upper gastrointestinal bleeding in emergency department patients.
The potential advantages of video capsule endoscopy over traditional endoscopy could include immediate availability, avoidance of sedation, patient tolerance, and the ability to rule out active bleeding in the emergency department.
The device used was the PillCam ESO2 – shown here in this animation:
Further research is needed. These small interesting studies demonstrate the potential for this imaging technology to be used in stable patients presenting to emergency departments. Since it can only diagnose rather than treat, it would not appear to have any role in unstable patients.
Video capsule endoscopy in the emergency department: a prospective study of acute upper gastrointestinal hemorrhage.
Ann Emerg Med. 2013 Apr;61(4):438-443
[EXPAND Abstract]
STUDY OBJECTIVE: Video capsule endoscopy has been used to diagnose gastrointestinal hemorrhage and other small bowel diseases but has not been tested in an emergency department (ED) setting. The objectives in this pilot study are to demonstrate the ability of emergency physicians to detect blood in the upper gastrointestinal tract with capsule endoscopy after a short training period, measure ED patient acceptance of capsule endoscopy, and estimate the test characteristics of capsule endoscopy to detect acute upper gastrointestinal hemorrhage.
METHODS: During a 6-month period at a single academic hospital, eligible patients underwent video capsule endoscopy (Pillcam Eso2; Given Imaging) in the ED. Video images were reviewed by 4 blinded physicians (2 emergency physicians with brief training in capsule endoscopy interpretation and 2 gastroenterologists with capsule endoscopy experience).
RESULTS: A total of 25 subjects with acute upper gastrointestinal hemorrhage were enrolled. There was excellent agreement between gastroenterologists and emergency physicians for the presence of fresh or coffee-ground blood (0.96 overall agreement; κ=0.90). Capsule endoscopy was well tolerated by 96% of patients and showed an 88% sensitivity (95% confidence interval 65% to 100%) and 64% specificity (95% confidence interval 35% to 92%) for the detection of fresh blood. Capsule endoscopy missed 1 bleeding lesion located in the postpyloric region, which was not imaged because of expired battery life.
CONCLUSION: Video capsule endoscopy is a sensitive way to identify upper gastrointestinal hemorrhage in the ED. It is well tolerated and there is excellent agreement in interpretation between gastroenterologists and emergency physicians.
[/EXPAND]
Capsule endoscopy in acute upper gastrointestinal hemorrhage: a prospective cohort study
Endoscopy. 2013 Jan;45(1):12-9
[EXPAND Abstract]
BACKGROUND AND STUDY AIMS: Capsule endoscopy may play a role in the evaluation of patients presenting with acute upper gastrointestinal hemorrhage in the emergency department.
METHODS: We evaluated adults with acute upper gastrointestinal hemorrhage presenting to the emergency departments of two academic centers. Patients ingested a wireless video capsule, which was followed immediately by a nasogastric tube aspiration and later by esophagogastroduodenoscopy (EGD). We compared capsule endoscopy with nasogastric tube aspiration for determination of the presence of blood, and with EGD for discrimination of the source of bleeding, identification of peptic/inflammatory lesions, safety, and patient satisfaction.
RESULTS:The study enrolled 49 patients (32 men, 17 women; mean age 58.3 ± 19 years), but three patients did not complete the capsule endoscopy and five were intolerant of the nasogastric tube. Blood was detected in the upper gastrointestinal tract significantly more often by capsule endoscopy (15 /18 [83.3 %]) than by nasogastric tube aspiration (6 /18 [33.3 %]; P = 0.035). There was no significant difference in the identification of peptic/inflammatory lesions between capsule endoscopy (27 /40 [67.5 %]) and EGD (35 /40 [87.5 %]; P = 0.10, OR 0.39 95 %CI 0.11 - 1.15). Capsule endoscopy reached the duodenum in 45 /46 patients (98 %). One patient (2.2 %) had self-limited shortness of breath and one (2.2 %) had coughing on capsule ingestion.
CONCLUSION:In an emergency department setting, capsule endoscopy appears feasible and safe in people presenting with acute upper gastrointestinal hemorrhage. Capsule endoscopy identifies gross blood in the upper gastrointestinal tract, including the duodenum, significantly more often than nasogastric tube aspiration and identifies inflammatory lesions, as well as EGD. Capsule endoscopy may facilitate patient triage and earlier endoscopy, but should not be considered a substitute for EGD.
[/EXPAND]
Echo for cardiac arrest outcome prediction
![]() A meta-analysis of studies evaluation transthoracic echo as a means of predicting return of spontaneous circulation in cardiac arrest (ROSC) provides some likelihood ratios to what we already know: absence of sonographic cardiac activity means a very low chance of ROSC.
A meta-analysis of studies evaluation transthoracic echo as a means of predicting return of spontaneous circulation in cardiac arrest (ROSC) provides some likelihood ratios to what we already know: absence of sonographic cardiac activity means a very low chance of ROSC.
The authors report a pooled negative LR of 0.18 (95% CI = 0.10 to 0.31), and a positive likelihood ratio of 4.26 (95% CI = 2.63 to 6.92).
They conclude that focused transthoracic echo is a fairly effective (although not definitive) test for predicting death if no cardiac activity is noted during resuscitation, and recommend interpreting the echo in the light of the test characteristics and the clinical pre-test probability, as one should do for all imaging investigations:
“An elderly patient with an unwitnessed cardiac arrest already has very poor odds for survival. Confirmation of asystole on echo lowers those pretest odds by a factor of 5.6 and therefore might lead to termination of resuscitation. However, in the case of a 50-year-old rescued from drowning, detection of cardiac contractility on echo would increase his already fair odds of survival by a factor of 4.3, prompting continued aggressive resuscitation.”
Only five relatively small studies contributed to the findings. A more definitive answer to this question should be provided in the future by the multi-centre REASON 1 trial.
Objectives: The objective was to determine if focused transthoracic echocardiography (echo) can be used during resuscitation to predict the outcome of cardiac arrest.
Methods: A literature search of diagnostic accuracy studies was conducted using MEDLINE via PubMed, EMBASE, CINAHL, and Cochrane Library databases. A hand search of references was performed and experts in the field were contacted. Studies were included for further appraisal and analysis only if the selection criteria and reference standards were met. The eligible studies were appraised and scored by two independent reviewers using a modified quality assessment tool for diagnostic accuracy studies (QUADAS) to select the papers included in the meta-analysis.
Results: The initial search returned 2,538 unique papers, 11 of which were determined to be relevant after screening criteria were applied by two independent researchers. One additional study was identified after the initial search, totaling 12 studies to be included in our final analysis. The total number of patients in these studies was 568, all of whom had echo during resuscitation efforts to determine the presence or absence of kinetic cardiac activity and were followed up to determine return of spontaneous circulation (ROSC). Meta-analysis of the data showed that as a predictor of ROSC during cardiac arrest, echo had a pooled sensitivity of 91.6% (95% confidence interval [CI] = 84.6% to 96.1%), and specificity was 80.0% (95% CI = 76.1% to 83.6%). The positive likelihood ratio for ROSC was 4.26 (95% CI = 2.63 to 6.92), and negative likelihood ratio was 0.18 (95% CI = 0.10 to 0.31). Heterogeneity of the results (sensitivity) was nonsignificant (Cochran’s Q: χ(2) = 10.63, p = 0.16, and I(2) = 34.1%).
Conclusions: Echocardiography performed during cardiac arrest that demonstrates an absence of cardiac activity harbors a significantly lower (but not zero) likelihood that a patient will experience ROSC. In selected patients with a higher likelihood of survival from cardiac arrest at presentation, based on established predictors of survival, echo should not be the sole basis for the decision to cease resuscitative efforts. Echo should continue to be used only as an adjunct to clinical assessment in predicting the outcome of resuscitation for cardiac arrest.
Bedside Focused Echocardiography as Predictor of Survival in Cardiac Arrest Patients: A Systematic Review
Acad Emerg Med. 2012 Oct;19(10):1119-1126
Needle decompression: it's still not going to work
![]() A pet topic that keeps coming up here is management of tension pneumothorax. Plenty of studies demonstrate that traditionally taught needle thoracostomy may fail, and open, or ‘finger’ thoracostomy is recommended for the emergency management of tension pneumothorax in a patient who is being ventilated with positive pressure (including those patients in cardiac arrest).
A pet topic that keeps coming up here is management of tension pneumothorax. Plenty of studies demonstrate that traditionally taught needle thoracostomy may fail, and open, or ‘finger’ thoracostomy is recommended for the emergency management of tension pneumothorax in a patient who is being ventilated with positive pressure (including those patients in cardiac arrest).
A recent CT scan-based study of adult trauma patients makes the case that needle decompression with a standard iv cannula would be expected to fail in 42.5% of cases at the second intercostal space (ICS) compared with 16.7% at the fifth ICS at the anterior axillary line (AAL).
The authors add an important point: “As BMI increases, there is a stepwise increase in chest wall thickness, further compounding the difficulty of needle placement in all but the lowest BMI quartile for the second ICS.”
An accompanying editorial cautions that the proximity of the heart may confer a safety issue if a needle is inserted blindly into the left 5th ICS at the AAL.
Objective To compare the distance to be traversed during needle thoracostomy decompression performed at the second intercostal space (ICS) in the midclavicular line (MCL) with the fifth ICS in the anterior axillary line (AAL).
Design Patients were separated into body mass index (BMI) quartiles, with BMI calculated as weight in kilograms divided by height in meters squared. From each BMI quartile, 30 patients were randomly chosen for inclusion in the study on the basis of a priori power analysis (n = 120). Chest wall thickness on computed tomography at the second ICS in the MCL was compared with the fifth ICS in the AAL on both the right and left sides through all BMI quartiles.
Setting Level I trauma center.
Patients Injured patients aged 16 years or older evaluated from January 1, 2009, to January 1, 2010, undergoing computed tomography of the chest.
Results A total of 680 patients met the study inclusion criteria (81.5% were male and mean age was 41 years [range, 16-97 years]). Of the injuries sustained, 13.2% were penetrating, mean (SD) Injury Severity Score was 15.5 (10.3), and mean BMI was 27.9 (5.9) (range, 15.4-60.7). The mean difference in chest wall thickness between the second ICS at the MCL and the fifth ICS at the AAL was 12.9 mm (95% CI, 11.0-14.8; P < .001) on the right and 13.4 mm (95% CI, 11.4-15.3; P < .001) on the left. There was a stepwise increase in chest wall thickness across all BMI quartiles at each location of measurement. There was a significant difference in chest wall thickness between the second ICS at the MCL and the fifth ICS at the AAL in all quartiles on both the right and the left. The percentage of patients with chest wall thickness greater than the standard 5-cm decompression needle was 42.5% at the second ICS in the MCL and only 16.7% at the fifth ICS in the AAL.
Conclusions In this computed tomography–based analysis of chest wall thickness, needle thoracostomy decompression would be expected to fail in 42.5% of cases at the second ICS in the MCL compared with 16.7% at the fifth ICS in the AAL. The chest wall thickness at the fifth ICS AAL was 1.3 cm thinner on average and may be a preferred location for needle thoracostomy decompression.
Radiologic evaluation of alternative sites for needle decompression of tension pneumothorax
Arch Surg. 2012 Sep 1;147(9):813-8
Echocardiography in Pulmonary Embolism
I had great fun joining in a Google Hangout with the Ultrasound Podcast guys and some real masters of emergency/critical care ultrasound. You can watch it here:
Is it time to abandon plain radiography in the trauma room?
 For patients who will be having a chest CT, perhaps sonography could replace chest radiography in the resus room as the initial imaging step; this recent prospective study shows its superiority over the ‘traditional’ ATLS approach.
For patients who will be having a chest CT, perhaps sonography could replace chest radiography in the resus room as the initial imaging step; this recent prospective study shows its superiority over the ‘traditional’ ATLS approach.
In haemodynamically stable patients with prophylactic pelvic splints in place, one could easily argue against plain pelvis films too (the caveat being rapid access to CT is necessary). The arguments against resus-room lateral cervical spine x-rays were made ages ago and these are now rarely done in the UK & Australia.
Is it time to abandon plain radiography altogether for stable major trauma patients?
Background: The accuracy of combined clinical examination (CE) and chest radiography (CXR) (CE + CXR) vs thoracic ultrasonography in the acute assessment of pneumothorax, hemothorax, and lung contusion in chest trauma patients is unknown.
Methods: We conducted a prospective, observational cohort study involving 119 adult patients admitted to the ED with thoracic trauma. Each patient, secured onto a vacuum mattress, underwent a subsequent thoracic CT scan after first receiving CE, CXR, and thoracic ultrasonography. The diagnostic performance of each method was also evaluated in a subgroup of 35 patients with hemodynamic and/or respiratory instability.
Results: Of the 237 lung fields included in the study, we observed 53 pneumothoraces, 35 hemothoraces, and 147 lung contusions, according to either thoracic CT scan or thoracic decompression if placed before the CT scan. The diagnostic performance of ultrasonography was higher than that of CE + CXR, as shown by their respective areas under the receiver operating characteristic curves (AUC-ROC): mean 0.75 (95% CI, 0.67-0.83) vs 0.62 (0.54-0.70) in pneumothorax cases and 0.73 (0.67-0.80) vs 0.66 (0.61-0.72) for lung contusions, respectively (all P < .05). In addition, the diagnostic performance of ultrasonography to detect pneumothorax was enhanced in the most severely injured patients: 0.86 (0.73-0.98) vs 0.70 (0.61-0.80) with CE + CXR. No difference between modalities was found for hemothorax.
Conclusions: Thoracic ultrasonography as a bedside diagnostic modality is a better diagnostic test than CE and CXR in comparison with CT scanning when evaluating supine chest trauma patients in the emergency setting, particularly for diagnosing pneumothoraces and lung contusions.
Diagnostic accuracy of ultrasonography in the acute assessment of common thoracic lesions after trauma
Chest. 2012 May;141(5):1177-83
Spinal imaging for the adult obtunded blunt trauma patient
‘You can’t clear the cervical spine until the patient wakes up!’ How often have you heard this said about a patient with severe traumatic brain injury who may not ‘wake up’ for weeks, if at all?
A controversial area, but many institutions now allow collar removal if a neck CT scan is normal. Does this rule out injury with 100% sensitivity? No – but it probably pushes the balance of risk towards removing the collar – an intervention with no evidence for benefit and plenty of reasons why it may be harmful to ventilated ICU patients. For example, clearing the cervical spine based on MDCT was associated with less delirium and less ventilator associated pneumonia, both of which have been associated with increased mortality in critically ill patients (this is referenced in the paper below).
The UK’s Intensive Care Society has had pragmatic guidelines along these lines since 2005, which can be found here. This month’s Intensive Care Medicine publishes an updated literature review providing some further support to this approach.
PURPOSE: Controversy exists over how to ‘clear’ (we mean enable the clinician to safely remove spinal precautions based on imaging and/or clinical examination) the spine of significant unstable injury among clinically unevaluable obtunded blunt trauma patients (OBTPs). This review provides a clinically relevant update of the available evidence since our last review and practice recommendations in 2004.
METHODS: Medline, Embase. Google Scholar, BestBETs, the trip database, BMJ clinical evidence and the Cochrane library were searched. Bibliographies of relevant studies were reviewed.
RESULTS: Plain radiography has low sensitivity for detecting unstable spinal injuries in OBTPs whereas multidetector-row computerised tomography (MDCT) approaches 100%. Magnetic resonance imaging (MRI) is inferior to MDCT for detecting bony injury but superior for detecting soft tissue injury with a sensitivity approaching 100%, although 40% of such injuries may be stable and ‘false positive’. For studies comparing MDCT with MRI for OBTPs; MRI following ‘normal’ CT may detect up to 7.5% missed injuries with an operative fixation in 0.29% and prolonged collar application in 4.3%. Increasing data is available on the complications associated with prolonged spinal immobilisation among a population where a minority have an actual injury.
CONCLUSIONS: Given the variability of screening performance it remains acceptable for clinicians to clear the spine of OBTPs using MDCT alone or MDCT followed by MRI, with implications to either approach. Ongoing research is needed and suggestions are made regarding this. It is essential clinicians and institutions audit their data to determine their likely screening performances in practice.
Clinical review: spinal imaging for the adult obtunded blunt trauma patient: update from 2004
Intensive Care Med. 2012 Mar 10. [Epub ahead of print]
Ultrasound for pneumonia
Lung ultrasound done by a single keen individual had better test characteristics than CXR in diagnosing pneumonia as defined by discharge diagnosis.
The lung ultrasound was considered to be positive for pneumonia if it showed consolidation (including air bronchograms) or a focal interstitial syndrome (localised increased density of ‘B’ lines)
Objective The aim of this study was to evaluate the diagnostic accuracy of bedside lung ultrasound and chest radiography (CXR) in patients with suspected pneumonia compared with CT scan and final diagnosis at discharge.
Design A prospective clinical study.
Methods Lung ultrasound and CXR were performed in sequence in adult patients admitted to the emergency department (ED) for suspected pneumonia. A chest CT scan was performed during hospital stay when clinically indicated.
Results 120 patients entered the study. A discharge diagnosis of pneumonia was confirmed in 81 (67.5%). The first CXR was positive in 54/81 patients (sensitivity 67%; 95% CI 56.4% to 76.9%) and negative in 33/39 (specificity 85%; 95% CI 73.3% to 95.9%), whereas lung ultrasound was positive in 80/81 (sensitivity 98%; 95% CI 93.3% to 99.9%) and negative in 37/39 (specificity 95%; 95% CI 82.7% to 99.4%). A CT scan was performed in 30 patients (26 of which were positive for pneumonia); in this subgroup the first CXR was diagnostic for pneumonia in 18/26 cases (sensitivity 69%), whereas ultrasound was positive in 25/26 (sensitivity 96%). The feasibility of ultrasound was 100% and the examination was always performed in less than 5 min.
Conclusions Bedside chest ultrasound is a reliable tool for the diagnosis of pneumonia in the ED, probably being superior to CXR in this setting. It is likely that its wider use will allow a faster diagnosis, conducive to a more appropriate and timely therapy.
Lung ultrasound is an accurate diagnostic tool for the diagnosis of pneumonia in the emergency department
Emerg Med J. 2012 Jan;29(1):19-23
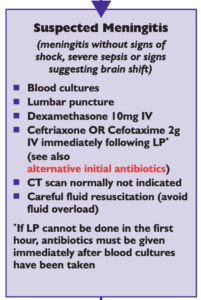
Offensive medicine: CT before LP
I’m getting worn down by clinicians – often other specialists – who insist that CT imaging of the brain is mandatory prior to lumbar puncture in all patients. There is surely a subgroup of patients (especially young ones) in whom the benefit:harm balance of CT comes out in favour of NOT doing the imaging. In these cases, getting the scan is not ‘defensive medicine’ but ‘offensive medicine’ – offending the principle of primum non nocere. During ED shifts I have recently had to perform online searches in order to furnish colleagues and patients’ medically qualified relatives with printouts of the literature on this. This page is here to save me having to repeat those searches. Regarding the practice of performing a routine head CT prior to lumbar puncture to rule out risk of herniation:
- Mass effect on CT does not predict herniation
- Lack of mass effect on CT does not rule out raised ICP or herniation
- Herniation has occurred in patients who did not undergoing lumbar puncture because of CT findings
- Clinical predictors of raised ICP are more reliable than CT findings
- CT may delay diagnosis and treatment of meningitis
- Even in patients in whom LP may be considered contraindicated (cerebral abscess, mass effect on CT), complications from LP were rare in several studies
Best practice, it would seem, is the following
- If you think CT will show a cause for the headache, do a CT
- If a CT is indicated for other reasons (depressed conscious level, focal neurology), do a CT
- If a GCS 15 patient is to undergo LP for suspected (or to rule out) meningitis, and they have a normal neurological exam (including fundi), and are not elderly or immunosuppressed, there is no need to do a CT first.
- If you’re seriously worried about meningitis and are intent on getting a CT prior to LP, don’t let the imaging delay antimicrobial therapy.
Here are some useful references:
1. The CT doesn’t help
CT head before lumbar puncture in suspected meningitis BestBET evidence summary: In cases of suspected meningitis it is very unlikely that patients without clinical risk factors (immunocompromise/ history of CNS disease/seizures) or positive neurological findings will have a contraindication to lumbar puncture on their CT scan If CT scan is deemed to be necessary, administration of antibiotics should not be delayed. BestBETS website
Computed Tomography of the Head before Lumbar Puncture in Adults with Suspected Meningitis Much cited NEJM paper from 2001 which concludes: “In adults with suspected meningitis, clinical features can be used to identify those who are unlikely to have abnormal findings on CT of the head” N Engl J Med. 2001 Dec 13;345(24):1727-33 Full Text
Cranial CT before Lumbar Puncture in Suspected Meningitis Correspondence in 2002 NEJM including study of 75 patients with pneumococcal meningitis: CT cannot rule out risk of herniation Cranial CT before Lumbar Puncture in Suspected Meningitis N Engl J Med. 2002 Apr 18;346(16):1248-51 Full Text
2. The CT may harm
Cancer risk from CT Paucis verbis card, from the wonderful Academic Life in EM
3. Guidelines say CT is not always needed
National (UK) guidelines on meningitis (community acquired meningitis in the immunocompetent host) available from meningitis.org. , including this box:
Practice Guidelines for the Management of Bacterial Meningitis These 2004 guidelines from the Infectious Diseases Society of America provide the following table listing the recommended criteria for adult patients with suspected bacterial meningitis who should undergo CT prior to lumbar puncture:
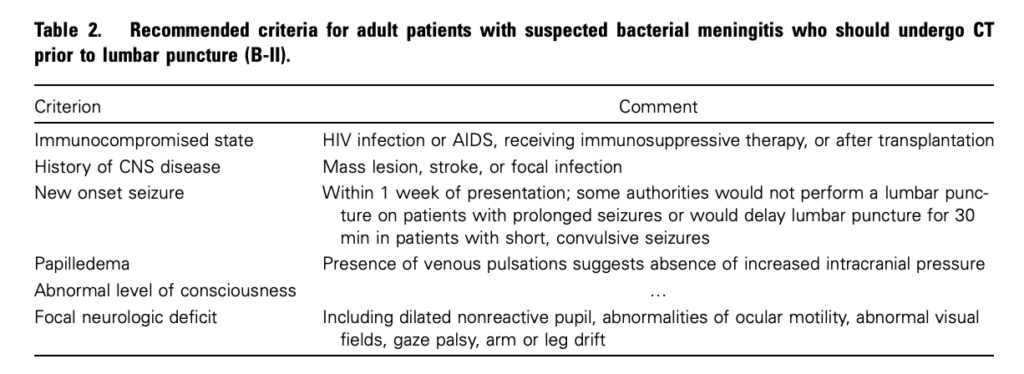
Clin Infect Dis. (2004) 39 (9): 1267-1284 Full text
4. This is potentially even more of an issue with paediatric patients
Fatal Lumbar Puncture: Fact Versus Fiction—An Approach to a Clinical Dilemma
An excellent summary of the above mentioned issues presented in a paediatric context, including the following:
On initial consideration a cranial CT would seem to be an appropriate and potentially useful diagnostic study for confirming the diagnosis of cerebral herniataion. The fallacy in this assessment has been emphasized by the finding that no clinically significant CT abnormalities are found that are not suspected on clinical assessments. Further, as previously noted, a normal CT examination may be found at about the time of a fatal herniation. Thus, the practical usefulness of a cranial CT in the majority of pediatric patients is limited to those rare patients whose increased ICP is secondary to mass lesions, not in the initial approach to acute meningitis.
Pediatrics. 2003 Sep;112(3 Pt 1):e174-6 Full Text
The last words should go to Dr Brad Spellberg, who in response to the IDSA’s guidelines wrote an excellent letter summarising much of the evidence at the time, confessed:
Why do we persist in using the CT scan for this purpose, despite the lack of supportive data? I am as guilty of this practice as anyone else, and the reason is simple: I am a chicken.
Early CT may rule out subarachnoid haemorrhage

A multicentre Canadian study challenges the practice of routine lumbar puncture after negative CT in patients with suspected subarachnoid haemorrhage. CT scanning within six hours was highly sensitive, although a few cases of initially misinterpreted CTs “illustrate the importance of having a qualified radiologist with a high level of skill interpreting the head scans in a timely manner“.
Nearly 2% of patients were lost to all follow-up; the authors point out that even if a quarter of these patients could have experienced a subarachnoid haemorrhage, the corresponding negative likelihood ratio for a computed tomography performed within six hours rises to only 0.024 (0.007 to 0.07). They assert:
Such a likelihood ratio could be incorporated into the informed discussion surrounding the risks and benefits of lumbar puncture after negative results on computed tomography for this diagnosis
They point out that when CT imaging is obtained more than six hours after headache onset, clinicians should continue to be cautious because of the decreasing sensitivity for subarachnoid haemorrhage beyond this time.
Objective To measure the sensitivity of modern third generation computed tomography in emergency patients being evaluated for possible subarachnoid haemorrhage, especially when carried out within six hours of headache onset.
Design Prospective cohort study. Setting 11 tertiary care emergency departments across Canada, 2000-9.
Participants Neurologically intact adults with a new acute headache peaking in intensity within one hour of onset in whom a computed tomography was ordered by the treating physician to rule out subarachnoid haemorrhage.
Main outcome measures Subarachnoid haemorrhage was defined by any of subarachnoid blood on computed tomography, xanthochromia in cerebrospinal fluid, or any red blood cells in final tube of cerebrospinal fluid collected with positive results on cerebral angiography.
Results Of the 3132 patients enrolled (mean age 45.1, 2571 (82.1%) with worst headache ever), 240 had subarachnoid haemorrhage (7.7%). The sensitivity of computed tomography overall for subarachnoid
haemorrhage was 92.9% (95% confidence interval 89.0% to 95.5%), the specificity was 100% (99.9% to 100%), the negative predictive value was 99.4% (99.1% to 99.6%), and the positive predictive value was 100% (98.3% to 100%). For the 953 patients scanned within six hours of headache onset, all 121 patients with subarachnoid haemorrhage were identified by computed tomography, yielding a sensitivity of 100% (97.0% to 100.0%), specificity of 100% (99.5% to 100%), negative predictive value of 100% (99.5% to 100%), and positive predictive value of 100% (96.9% to 100%).
Conclusion Modern third generation computed tomography is extremely sensitive in identifying subarachnoid haemorrhage when it is carried out within six hours of headache onset and interpreted by a qualified radiologist
Sensitivity of computed tomography performed within six hours of onset of headache for diagnosis of subarachnoid haemorrhage: prospective cohort study
BMJ. 2011 Jul 18;343:d4277
